Department of Physiatry
The physiatrists at Hospital for Special Surgery perform non-operative treatment procedures on patients who have spinal and sports-related injuries as well as other musculoskeletal problems. These procedures are combined with medically supervised exercise therapies to restore mobility and function in patients who might otherwise require surgery.
Several members of the Department of Physiatry also perform electrodiagnostic studies such as nerve conduction and electromyography. These diagnostic studies help to determine whether patients may have nerve or muscular disorders such as lumbar or cervical radiculopathy, carpal tunnel syndrome, and other debilitating conditions.
The Department is not only involved with the development of new non-invasive procedures, it also employs innovative research techniques to better understand and validate many non-operative or minimally invasive interventional procedures to treat spinal and sports-related injuries.
What is Physiatry?
Physiatry – also known as physical medicine and rehabilitation (PM&R) – is a medical specialty focused on the nonsurgical treatment of musculoskeletal conditions that cause pain and/or physical weakness. Physiatry first emerged as a medical specialty shortly after World War II, when veterans returned with spinal cord injuries, traumatic brain injuries, loss of limbs and other musculoskeletal impairments. The specialists who emerged from this specialty are called physiatrists and they combine their knowledge of anatomy and biomechanics with the goal of restoring function to individuals with these types of injuries.
When should I see a physiatrist?
Many people who experience pain or dysfunction in their bones, joints or soft tissues are confused about which type of medical specialist is appropriate for them. The trend in medicine toward specialization had made this an increasingly difficult task. People wonder, “Do I have a serious condition that requires surgery or will simple rest and exercise can fix the problem?” In many cases, especially when a spine injury is suspected, a physiatrist is the appropriate doctor who can help treat or determine the appropriate level of care.
Regardless of which type of practitioner you consult first, people who think they may have a bone or joint injury of any kind should find a doctor at an institution that emphasizes collaboration among disciplines and which specializes in every aspect of musculoskeletal treatment and recovery. Patients with a musculoskeletal injury can be assured that at HSS, non-operative care is provided whenever possible and appropriate.
Read more about What is a Physiatrist?
How do I find the right specialist?
Not everyone necessarily needs to see a physician or a surgeon for their first visit. Although HSS is well-known for orthopedic surgery, the majority of our outpatient visits result in nonsurgical, medical and rehabilitative care. All medical and surgical departments at HSS share the goal for each patients to see the right practitioner for the right treatment at the right time.
The Department of Physiatry places a strong emphasis on triage – a process in which the severity of a condition and the urgency of treatment is assessed – and on facilitating access to appropriate care. With proper assessment by a nurse practitioner or a physical therapist, the patient can often get the attention he or she needs promptly. This is also the best way to avoid progression to a chronic problem or one that is more difficult to treat.
To illustrate how HSS determines the right path of care, these are three hypothetical scenarios in which a person might contact the Hospital to seek treatment for back pain.
- Directly. A person calls or books online directly with a specific physician or surgeon of their choosing.
- Referral. An individual is referred by a health care provider (physical therapist, nurse clinician or primary care doctor) who believes that they should see a specialist or requires surgery.
- Unsure. A person has just experienced the acute onset of back pain or sustained a back injury and does not know what kind of treatment they require from a spine specialist.
HSS has many ways to help the unsure person get immediate care by booking online or speaking to one of our physician referral specialists. Depending on the nature and severity of the injury, a spine specialist will then determine if the patient needs immediate referral to a physiatrist or to a different specialist.
HSS Direct Access for patients
Another option is the Direct Access Physical Therapy program. Experienced physical therapists, who have already passed rigorous qualifying tests for certification, can diagnose and treat a patient without a doctor’s prescription.If needed, they can escalate the care to a physiatrist or other appropriate specialist.
Regardless of the path, once treated, the patient's progress is tracked continually by the spine specialist. If the patient achieves relief, then the focus of treatment turns to prevention. If not, then the spine specialist ensures that the patient receives the next level of care as appropriate for the injury or disorder. After the patient has recovered, HSS specialists provide direction on maintaining wellness.
Integrated Care and Research
At HSS, collaboration between physiatry and other orthopedic specialties is easier because oftentimes, they are under the same roof. If a physiatrist believes a patient is in need of surgery, a simple referral to one of the surgeon's at the same location can be made, and vice versa. This arrangement allows for an easy transition for patients and improved communication among physicians.
In addition to acting as partners with other specialists in the delivery of care, HSS physiatrists take an active role in collaborative research, such as conducting surveys to clearly identify patient expectations and goals of care. Areas of study include regenerative medicine, a discipline in which platelet-rich plasma, bone morphogenic proteins and/or stem cells may be used to repair and restore damaged and diseased musculoskeletal tissue.
HSS research teams include members of multiple departments in order to bring together different points of view, which then increases the understanding of what the research shows and which patients may potentially benefit from it.
Meet the Team

Collaborations
HSS is collaborating with the following healthcare organizations to bring world-class musculoskeletal care to patients in South Florida.
For Patients
The Department provides over 30,000 ambulatory care visits a year, including approximately 3,900 minimally invasive procedures and 1,100 EMG/NCV studies, attending over 17,500 returning patients and 7,500 new patients each year.
The following is a partial list of procedures performed by physiatrists at HSS:
- IntraDiscal Electrothermal Therapy (IDET) is a minimally invasive procedure that offers an important treatment option to individuals with lower back pain caused by lumbar disc disease. The physician then passes a thermal catheter through the needle and into the injured disc in the specific area of the annulus tear. The catheter heats the collagen of the disc to shrink the protruded material and destroy the pain fibers
- Epidural steroid injection is an umbrella term applying to a variety of techniques performed to deliver a corticosteroid preparation around a nerve exiting the spinal cord in an epidural space. This procedure decreases inflammation of the nerve roots, thereby reducing pain for several months and hopefully aiding the healing process as well.
- Nucleoplasty uses radiofrequency energy to treat patients with low back pain from contained, or mildly herniated, discs. Guided by X-ray imaging, a wand-like instrument is inserted through a needle into the disc to create a channel that allows inner disc material to be removed. The wand then heats and shrinks the tissue, sealing the disc wall. Several channels are made, depending on how much disc material needs to be removed.
- Radiofrequency ablation uses high-frequency alternating current flow to generate heat and destroy pain sensing nerves. A narrow electrode is introduced to the affected nerve. Precisely controlled generator heat is generated to destroy the nerve.
- Nerve conduction/electromyography testing, or EMG testing, is a two-part electrodiagnostic test that is used to study nerve and muscle function, and it can provide your doctor with specific information about the extent of nerve and/or muscle injury. The test consists of a nerve conduction study and a needle exam for muscle testing. The nerve conduction study entails stimulating the nerves at different points with small electric shocks, artificially activating them so their function can be measured. The needle exam involves inserting very fine needles into several muscles with determine normal and abnormal electrical signals given off by the muscles. EMG testing usually takes anywhere from 30 to 90 minutes, depending on the condition being tested and findings of the study.
- Joint lavage procedures are arthroscopic techniques essentially meant to wash loose tissue debris and inflammatory agents away from the interior of a major joint, such as the knee. Although the lavage procedure is a short-term solution, it may assist in relieving the symptoms of those suffering from osteoarthritis for a number of years. Joint injections are performed for diagnostic and therapeutic purposes, and they can be used in two ways - for aspiration, which involves removing fluid for testing or drainage, and fluid injection, whereby medications such as corticosteroids are injected into a joint to medicate areas affected by inflammatory arthritis.
Condition & Treatment Highlights
Fellowship Training
The Department provides a one-year Spine and Sports Medicine Fellowship, with four fellows accepted each year. Two fellows are ACGME accredited Primary Care Sports Medicine fellows and two are recognized by NASS. The fellowship program focuses on the comprehensive diagnosis and management of musculoskeletal conditions with a focus on Spine and Sports related conditions. This includes comprehensive radiology interpretation, biomechanical and functional assessments, diagnostic and therapeutic interventional spine procedures (cervical, thoracic and lumbar), diagnostic and interventional ultrasound, electrodiagnostics and regenerative medicine. There are daily didactics and a research requirement.
The Department also takes part in the training of Physical Medicine and Rehabilitation residents from New York-Presbyterian Hospital (Cornell/Columbia) and Rutgers (New Jersey Medical School/Kessler) residency programs and is involved in the education of medical students from Weill Cornell Medicine as well as visiting health profession students from across the globe.
Physiatrist Researchers
Research Staff
- Jennifer Cheng, PhD
- Olivia Leupold, BA
- Sophia Perez, BA
- Olivia Rau, BA
- SM Shariar, BS
Students and trainees who are interested in volunteering in research for our department may contact physiatryresearch@hss.edu.
Research Initiatives
The Physiatry Department is continuously exploring ways to improve established treatments and to research the safe and effective adoption of novel techniques. Our ultimate goal is to identify the ideal treatment paradigm for our patients.

Studies managed in 2024

Articles/chapters/abstracts published in 2024
Main Focus Areas of Research
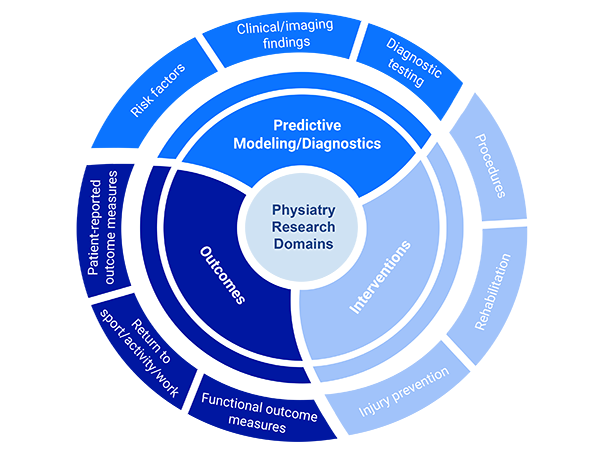
Predictive Modeling/Diagnostics
- Risk factors
- Clinical/imaging findings
- Diagnostic testing
Interventions
- Procedures
- Rehabilitation
- Injury prevention
Outcomes
- Patient-reported outcome measures
- Return to sport/activity/work
- Functional outcome measure
Many of our studies encompass more than one focus area of research and range from basic science to translation human to clinical trials. They are conducted in collaboration with intramural and extramural researchers in radiology, orthopedics, neurology, primary care sports medicine, laboratory/pathology/chemistry, and physical therapy.
Learn more about our currently active studies.
Research Highlights
Recent Publications
- Katz NB, Karnovsky SC, Robinson DM, DeLuca SE, Yun PH, Casey E, Wasfy MM, Tenforde AS. Sex differences and extracorporeal shockwave therapy outcomes in runners with Achilles or hamstring tendinopathy. J Clin Med. 2024 Dec 3.
- Leupold O, Cheng J, Wimberly A, Nguyen J, Tilley D, Gabbett TJ, Casey E. A novel approach for monitoring training load and wellness in women’s college gymnastics. Sports Health. 2024.
- Malik GR, Cheng J, Rothman R, Leupold O, Jawetz S, Prather H. Characterization and variability of PROMIS-10 scores in knee osteoarthritis based on severity and number of compartments involved: a retrospective review. Accepted for publication in PM&R on Oct 3, 2024.
- Shetty KD, Basu AR, Nuckols TK; Multi‐Society Working Group for Electrodiagnosis Quality Measures in CTS, Feinberg JH. Refining quality measures for electrodiagnostic testing in suspected carpal tunnel syndrome to account for acceptable variations in practice: Expert review process. Muscle Nerve. 2024 Sep;70(3):316-324.
- Schneider R, Cheng J, Hannafin J, Wyss J. Letter to the Editor regarding “Hydrodilatation versus corticosteroid injection in treatment for adhesive capsulitis” by Latzka et al. PM&R. 2024 Sep 20.
- Solomon S, Lin S, Prather H, Hunt DM, Agarwal M, Bloom NJ, Mills L, Clohisy JC, Harris-Hayes M. Low back pain or injury before collegiate athletics, a potential risk factor for non-contact injuries. J Athl Train. 2024 Sep 17.
- Casey E, Patel TS, Almedia JF, Binder J, Bucke J, Duffy K, Faustin M, Iwasaki Y, Kruse D, Laird J, Laury T, Mathieu JF, Rigg J, Tomlinson C, Thomas C, Stokes KA. Artistic gymnastics-specific extension of the IOC 2020 consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport. BMJ Open Sport Exerc Med. 2024;10:e002040.
- Campbell G, Tan ET, Lin Y, Akerman M, Milani CJ, Feinberg JH, Sneag DB. Longitudinal quantitative MRI changes of muscle denervation in Parsonage-Turner syndrome. J Magn Reson Imaging. 2024.
- Oleka CT, Anderson T, Ackerman KE, Elliott-Sale KJ, Kraus E, Casey E, Stellingwerff T, Donaldson AT, Finnoff JT, Post EG, Adams WM. An update to terminology describing abnormal uterine bleeding in female athletes: facilitating cross-disciplinary health care. Br J Sports Med. 2024 Jul 18.
- Cushman DM, Catalano E, Hoffman J, Casey E. Achilles tendon rupture preceded by normal asymptomatic imaging in a collegiate gymnast: a case report. Radiol Case Rep. 2024;19:3470-3472.
- McDougall A, McGowen S, Kirschner J. Evidence-based management of ulnar neuropathy at the elbow. Curr Phys Med Rehabil Rep. 2024 Jun 24.
- Rodriguez LA 2nd, Casey E, Crossley E, Williams N, Dhaher YY. The hormonal profile in women using oral contraceptives is not as stable as previously thought: a temporal analysis of serum endogenous and exogenous hormones. Am J Physiol Endocrinol Metab. 2024 May 22.
- Chan W, Rim F, Liu S, Jules-Elysee K, Liu J, Memtsoudis S, Sideris A. Inpatient dronabinol utilization: an institutional retrospective study to determine prevalence and indications for clinical application. Br J Anaesth. 2024 Apr 30.
- Prather H, Leupold O, Suter C, Mehta N, Griffin K, Pagba M, Hall K, Taverna-Trani A, Rose D, Jasphy L, Yu SX, Cushner F, Gonzalez Della Valle A, Cheng J. Early outcomes of orthopedic pre-surgical patients enrolled in an intensive, interprofessional lifestyle medicine program to optimize health. Am J Lifestyle Med. 2024 May 16.
- Afifi T, Barrack MT, Casey E, Huddle M, Kliethermes SA, Kraus E, Toresdahl BG, Wasfy MM, Tenforde AS. Infographic. Head to toe considerations for the postpartum endurance athlete. Br J Sports Med. 2024
Recent Abstracts Accepted or Presented at Conferences
- Prather H, Leupold O, Griffin K, Suter C, Pier B, Cheng J. Comparison of immediate surgical outcomes following participation in an intensive vs. selective lifestyle medicine program. ACLM Lifestyle Medicine Conference 2024.
- Prather H, Leupold O, Griffin K, Suter C, Pier B, Cheng J. Comparison of immediate surgical outcomes following participation in an intensive vs. selective lifestyle medicine program. NYP Rehabilitation Research Day 2024.
- Angelo N, Cheng J, Creighton A, Prather H. Patient characteristics and considerations in the use of platelet rich plasma in the management of high-grade gluteal tears. NYP Rehabilitation Research Day 2024.
- Deo P, Cheng J, Leupold O, Trotzky Z, Halvorsen H, Dela Torre K, Sink E, Prather H. Comparisons of the STaRT MSK tool to patient-reported outcome measures in patients with hip and pelvic girdle pain in the setting of acetabular hip dysplasia. NYP Rehabilitation Research Day 2024.
- Leupold O, Cheng J, Carrino J, Baxi N. Prevalence of carotid artery calcifications on cervical spine x-rays in a musculoskeletal patient population. NYP Rehabilitation Research Day 2024.
- Balkaran S, Vad V. Use of a novel far infrared ray emitting compression knee sleeve for the treatment of knee osteoarthritis. NYP Rehabilitation Research Day 2024.
- Casey E, Cheng J, Miranda D. Tracking training load & wellness in women’s artistic gymnastics: is the juice worth the squeeze? USA Gymnastics National Congress 2024.
Why choose HSS? Our patients say it best.
In the News
- Got neck pain? This is the kind of pillow that sleep specialists recommend
- HSS Experts Offer Tips to Prevent Golfer’s Elbow
- Rockettes x HSS: The Science Behind Injury Prevention & Athletic Training for the Christmas Spectacular
- Does Exercising in the Cold Increase My Risk of Injury?
- GLP-1s may have profound impact on total joint replacement
- Your big, cushy bed could be ruining your sleep. Time to rethink the floor
- What Runners Need to Know About Cycle Syncing and Performance
- Speaking Up About Pelvic Health
- The Best Mattress Toppers Are the Subtle Upgrade Your Bed Needs
- Why a tatami mat might help you sleep better
- HSS Experts Offer Tips To Prevent Back Injuries When Playing Golf
- How to Make Dancing in the Heat Less Miserable for Students
- A Legacy of Healing: HSS (Hospital for Special Surgery) Hosts its 40th Tribute Dinner
- Hospital for Special Surgery Announced as the Singlet Sponsor for Front Runners New York LGBT Pride Run
- HSS Honors Distinguished Physicians Todd Albert and Joel Press and HSS Chairman Emeritus Kendrick Wilson, III at Tribute Dinner
- Dr. Angelie Mascarinas a Physiatrist at HSS Florida joins ESPN West Palm Tonight
- 7 Best Big And Tall Office Chairs That Keep You Aligned And Supported
- Prioritizing Weight Loss With Obesity Can Improve Post-Op Results
- Turns Out, a Knee Pillow Might Be the Back Pain Fix You Need
- Nearly 1 in 4 U.S. Women Face Pelvic Floor Disorders, Highlighting the Need for Specialized Care
- HSS Lifestyle Medicine Program Improves Health Before Elective Orthopedic Surgery for Patients with Chronic Diseases
- More than Ozempic, American health care needs a lifestyle revolution
- Shoulder Pain Pointers for Primary Care
- Marathon Performance Tips from Hospital for Special Surgery- Nnaemeka Echebiri, MD
- Lifestyle medicine program improves musculoskeletal surgical outcomes
- 3 Ways to Make Your Commute Actually Enjoyable
- How To Prevent Tech Neck And Fix Your Posture For Good, According To Experts
- Hospital for Special Surgery Named Official Hospital and Partner of St. John’s University Athletics
- Choose Physiatry for Comprehensive Care of Sports and Spine Injuries
- 9 Best Mattresses for Stomach Sleepers in 2024
- Consulting a Physiatrist for Groin Pain
- From motherhood to medals: How Olympic moms return to competition
- This is why your back hurts—and how to relieve the pain
- Too Sore to Stroll? An MD Reveals How To Soothe Hip Joint Pain When Walking
- Walk Your Back Pain Away
- Study: This Simple Activity May Help Reduce Lower Back Pain
- How to Relieve Hip Pain
- Just Wondering: Is It Normal for My Bones To Crack *a Lot* When I Move?
- 8 Best Exercises for Lower Back Pain
- Experts Weigh In On The Best Sleeping Position For Your Health
- Golf Simulator Helps Injured Players Get Back on the Course
- WSJ: How to Choose a Mattress
- Sitting Like This Can Bring Major Health Benefits As You Age
- Is Every Desk Worker Going To Have A Dowager's Hump?
- The Best Shoes For Back Pain, According To Medical Experts
- Exercise and Strength Training With Arthritis
- Stretching studios are popping up everywhere. Are they worth it?
- HSS Celebrates Women’s History Month (Dr. Jennifer O’Connell)
- We Tested Over 50 Mattresses to Give You Better Rest—Here Are the Best Mattresses for Every Sleeper
- Understanding Pain