Cervical Radiculopathy
Nearly 10% of adults will experience some form of severe neck pain in any given calendar year. Most cases of neck pain have multiple causes, such as inflamed (swollen) muscles, ligaments, joints or nerves.

Often, inflammation occurs in all of these tissues at once, causing neck pain that may last from a few days to several weeks. Some neck pain, however, can persist for longer periods of time and may also radiate to the shoulder or arm. Neck pain that radiates to the arm or that is accompanied by feelings of numbness or weakness may be caused by cervical radiculopathy.
What is cervical radiculopathy?
Cervical radiculopathy is pain and neuropathy in the neck that results from a pinching or inflammation of a cervical nerve at the point where it exits the spine, called the foramen or neuroforamen.
The name radiculopathy is derived from a combination of the Latin word radicula (small root) and the Greek word pathos (disease). Cervical refers to the neck region of the spine. Radiculopathy of the lower back is known as lumbar radiculopathy and includes the condition commonly known as sciatica, which is the irritation of the sciatic nerve.
Spine anatomy: Vertebrae
The spine is not one long rigid bone. It consists of 24 small bones called vertebrae that are stacked in a column from the pelvis to the base of our skull. These bones connect to create a canal that protects the spinal cord.
The vertebrae are divided into four regions.
From top to bottom, these are:
- The cervical spine (the neck) – the first seven vertebrae located just below the skull
- The thoracic spine – the 12 vertebrae of the upper back
- The lumbar spine – the five vertebrae of the lower back
- The sacral spine – composed of a triangular structure called the sacrum (five individual vertebrae that fuse together between the age of 18 and 30) and the coccyx (commonly called the tailbone and composed of three to five individual vertebrae, some of which may fuse together in adulthood)
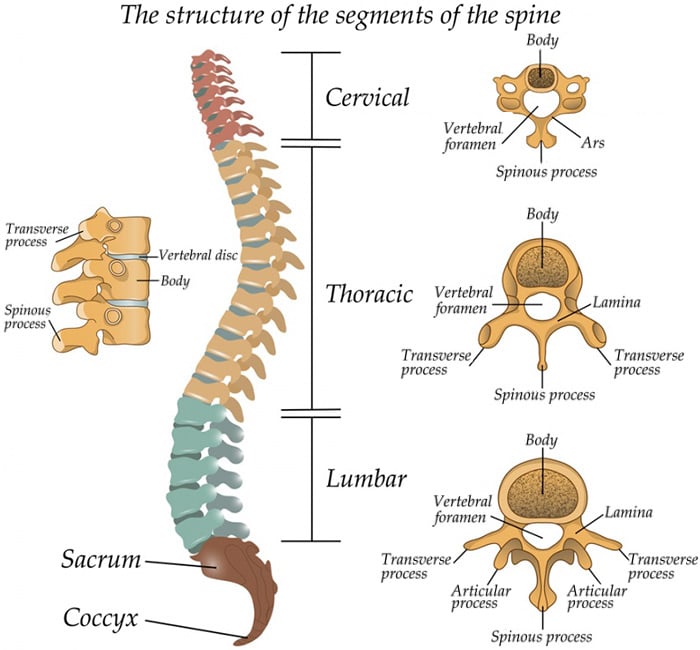
Lateral (side) view of the spine of a person facing left.
What causes cervical radiculopathy?
The most common conditions that cause cervical radiculopathy include:
- cervical disc herniation (herniated disc or "slipped disc")
- cervical spondylosis
Cervical disc herniation
A spinal disc is a spacer between each vertebra. The disc is actually a two-part structure. The circular outer layer, called the annulus, is tough and ligament-like. It encapsulates the soft, gel-like inner part, called the nucleus.
A gradual or severe, sudden tear of the annulus may allow changes in the outer contour of the disc to protrude like a pimple. While any slight protrusion of a disc is classified as a herniation, the most problematic ones are larger and more prominent over the passageway of a spinal nerve (called the nerve “root”).
Cervical spondylosis with radiculopathy
Cervical spondylosis refers to gradual wear and tear or age-related changes in the cervical spine. Such changes may include:
- narrowing of the disc space
- bulging of the contour of the disc
- calcification of the disc and vertebral margins that result in spurs
Disc herniation and cervical spondylosis conditions are both so-called "degenerative" processes – age-related changes of the spine that occur with aging and or wear and tear. They become more prevalent with age, and they are known to occur in individuals who experience no neck pain at all.
Since a herniated disc is a softer projection than spondylosis, it is more likely to become smaller or resolve completely on its own over time. Spondylosis, however, generally refers to harder bone “spurs.”
Studies have shown that a simple tally of the amount of degenerative change (commonly referred to as “arthritis”) in an individual’s spine is not a good predictor of how much neck pain a person will have. However, spurring or disc herniation that significantly narrows the nerve exit passage (foramen), a condition referred to as foraminal stenosis or neuroforaminal stenosis, may be identified as the culprit in specific episodes of cervical radiculopathy.
What are the symptoms of cervical radiculopathy?
Cervical radiculopathy symptoms primarily involve persistent neck pain that is accompanied by indicators of possible nerve root irritation, such as:
- pain that radiates down the arm or even to the hand
- numbness
- weakness
What does a pinched nerve in the neck feel like?
A pinched nerve in the neck (cervical nerve compression) can cause a variety of sensations. Most commonly, one may experience a sharp or burning feeling of pain that may radiate to the shoulder or the arm, and/or a tingling or “pins and needles” feeling associated with numbness.
How do you diagnose cervical radiculopathy?
A physician makes a diagnosis by learning the patient’s symptoms and history, conducting a physical exam, and then cross-referencing both with the results of appropriate radiological imaging.
Physical examination
Neck pain and arm pain can occur simultaneously or separately over the course of cervical radiculopathy. Your physician may attempt to provoke the pain by extending your neck and head backward. A careful physical examination may also detect:
- changes in reflexes
- patches of sensation loss
- specific muscle weakness resulting from the dysfunction of a cervical spinal nerve
Radiology findings
A conventional X-ray of the cervical spine may show the margins of the bony vertebra and bony spur formation in the area of the nerve foramen.
MRI or CT scans of the cervical spine show the spine in cross-section and from other angles. These imaging technologies can also provide views of the surrounding soft-tissue structures that are not visible on a conventional X-ray, such as the spinal discs and nerves.
A specific advantage of an MRI scan is that it may demonstrate some of the dynamic effects of ongoing metabolic stresses in specific body tissues, which may be causing pain symptoms. Different types of MRI scan sequences may highlight physiological events in the body that correlate with symptoms, such as:
- areas of swelling
- changing tissue consistency or blood flow
This helps doctors determine which problems are causing symptoms and which are common, age-related spine deformities that may not cause pain or other symptoms. For example, disc bulges and bone spurs often develop in later years, but do not always cause pain.
The presence and severity of disc herniations and foraminal stenosis can be more formally evaluated using these types of MRI scans. It is imperative, however, that the findings from such scans be correlated with the patient's symptoms and problems. Radiology spine reports can be alarming if they are misinterpreted. Something that looks menacing to the untrained eye may instead be as normal as the wrinkles on the aging skin.
What can make cervical radiculopathy worse?
If you have been diagnosed with cervical radiculopathy, various activities or even inactivity may be exacerbating your symptoms. These include work or sports activities that involve repetitive neck movements or heavy lifting. Other possible contributing factors include poor posture, sleeping ergonomics (pillow choice), continual emotional stress, and being overweight, all of which can put stress on your neck muscles and/or your cervical spine.
Does cervical radiculopathy require surgery?
Most patients recover with non-operative treatment. If pain continues in spite of these treatments for cervical radiculopathy, surgery, such as a spinal decompression procedure, may be recommended. Additionally, in those patients with especially severe cases of radiculopathy, surgical treatment at an earlier point in time may be appropriate.
What are the nonsurgical treatments for cervical radiculopathy?
There are several non-operative cervical radiculopathy treatment options, including:
- rest and immobilization of the neck
- medications
- physical therapy
- epidural steroid injection treatment
Medical research update: Using non-operative treatments as the standard of care for a pinched nerve in the neck is supported by a variety of scientific evidence. Numerous studies have shown that cervical radiculopathy usually improves with time without the need for surgery. One investigation summarized the findings of more than 1,200 previously published studies on cervical disc herniations treated without surgery. It demonstrated that the vast majority of patients had good results and symptom relief over the course of two to three years. Other studies of patients treated nonsurgically have shown that disc herniations visible on MRIs were shown to subside on repeated scans after a period of time.
Although numerous studies demonstrated good outcome results of nonsurgical therapies, there are far fewer studies that conclusively support the use of more intensive treatment by epidural steroid injections as the major reason for recovery. Many studies have reported good results using the epidural steroid injection procedure in patients who do not respond to initial therapies. But thorough studies with sufficiently large numbers of patients that utilize good randomization methods and follow-up are simply not available.
New studies have helped to refine the actual techniques and safety of these procedures. This includes the broader adoption of using radiologic guidance for injection procedures, improvements in the quality of fluoroscopic imaging tools, and recommendations on specific techniques for the procedures itself.
Rest and immobilization of the neck
During the acute phase of cervical radiculopathy, it may be important to refrain from repetitive movements of the neck, as well as forceful or heavy lifting movements. A soft cervical collar is often helpful for limiting neck motion and providing splinting for position of comfort when at rest.
Medications
Whenever possible, your physician may prescribe anti-inflammatory medication, particularly at the outset of the problem. Some radiculopathies will respond to nonsteroidal anti-inflammatory medications (NSAIDs) alone, but a short course of oral corticosteroid medication is often prescribed as well.
Medications that include gabapentin and pregabalin are frequently used to relieve radiculopathy related pain symptoms. These medications work differently than anti-inflammatory medications. (They are also used, though less frequently, for patients suffering seizure disorders.) In some cases, they may be more effective than other analgesic medications.
Physical therapy
The physical therapist can administer intermittent spinal traction to decompress the cervical vertebrae and help relieve pain. If traction is particularly effective, a patient can purchase a traction unit and self-administer traction at home on a regular basis, although it is important to do it after receiving guidance from your doctor or physical therapy. When pain is reduced, range of motion and strengthening exercises can help to gradually restore areas in the neck and shoulder that have been weakened by disuse and pain.
Various cervical radiculopathy exercises such as isometrics of the neck muscles, stretches and nerve gliding maneuvers may also help, but should only be performed as instructed by a healthcare provider to avoid possible injury that could worsen symptoms.
Epidural steroid injection treatment
In many cases, the above therapies for cervical radiculopathy are ineffective. Epidural steroid injections may benefit patients whose kind of lasting pain might otherwise require surgery. A transforaminal epidural injection procedure can be performed on an outpatient basis using fluoroscopy (real-time X-ray guidance). A trained specialist will use an MRI scan and physical exam to identify to suspected area of injury. Under fluoroscopic guidance, a needle is directed – in most cases under local anesthesia alone – to area of the pinched nerve.
Here is how it works: The membrane that covers the spine and nerve roots is called the dura. The space surrounding the dura is the epidural space. An epidural injection places anti-inflammatory medicine into the epidural space to decrease inflammation of the nerve roots. This reduces pain and hopefully aids in the healing process. The injection may provide permanent relief, it may provide temporary pain relief for several months while the underlying injury or cause is healing.
Improvement may occur immediately or within two weeks, depending on the patient and the cause of the radiculopathy. Some patients will respond after one injection, but others may require up to three, interspersed over the course of a recovery period of one to three months. Most patients will benefit from a gradual exercise program performed simultaneously with the direction and supervision of a physical therapist.

Figure 1: Model showing needle positioning for transforaminal epidural steroid injection.
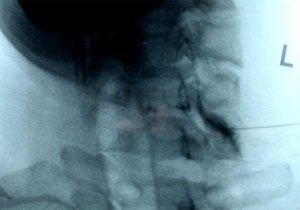
Figure 2: Fluoroscopic image of a Left C6/7 transforaminal epidural injection. Contrast solution outlines the epidural space and exiting cervical nerve root. Immediately afterwards, a solution of corticosteroid and local anesthetic were injected.
References
- Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Sep;72(8):1178-84. PMID: 2398088.
https://pubmed.ncbi.nlm.nih.gov/2398088/ - Boden SD. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. 2005.
- Bush K, Hillier S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996;5(5):319-25. doi: 10.1007/BF00304347. PMID: 8915637.
https://pubmed.ncbi.nlm.nih.gov/8915637/ - Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998 Aug 1;23(15):1689-98. doi: 10.1097/00007632-199808010-00015. PMID: 9704377.
https://pubmed.ncbi.nlm.nih.gov/9704377/ - Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine (Phila Pa 1976). 2001 Nov 15;26(22):2463-6. doi: 10.1097/00007632-200111150-00013. PMID: 11707711. https://pubmed.ncbi.nlm.nih.gov/11707711/
- Kobayashi N, Asamoto S, Doi H, Ikeda Y, Matusmoto K. Spontaneous regression of herniated cervical disc. Spine J. 2003 Mar-Apr;3(2):171-3. doi: 10.1016/s1529-9430(02)00556-9. PMID: 14589234. https://pubmed.ncbi.nlm.nih.gov/14589234/
- Liang L, Cui X, Feng M, Zhou S, Yin X, He F, Sun K, Yin H, Xie R, Zhang D, Zhou Y, Wu Y, Tan G, Wang Z, Wang X, Zhang J, Zhu L, Yu J, Wei X. The effectiveness of exercise on cervical radiculopathy: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2019 Aug;98(35):e16975. doi: 10.1097/MD.0000000000016975. PMID: 31464943; PMCID: PMC6736459.
https://pubmed.ncbi.nlm.nih.gov/31464943/ - Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. A randomized, double-blind, active control trial of fluoroscopic cervical interlaminar epidural injections in chronic pain of cervical disc herniation: results of a 2-year follow-up. Pain Physician. 2013 Sep-Oct;16(5):465-78. Erratum in: Pain Physician. 2013 Nov-Dec;16(6):609. https://pubmed.ncbi.nlm.nih.gov/24077193/
- Manchikanti L, Nampiaparampil DE, Candido KD, Bakshi S, Grider JS, Falco FJ, Sehgal N, Hirsch JA. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician. 2015 Jan-Feb;18(1):39-60. PMID: 25675059. https://pubmed.ncbi.nlm.nih.gov/25675059/
- Persson L, Anderberg L. Repetitive transforaminal steroid injections in cervical radiculopathy: a prospective outcome study including 140 patients. Evid Based Spine Care J. 2012 Aug;3(3):13-20. doi: 10.1055/s-0032-1327805. PMID: 23531493; PMCID: PMC3592766.
https://pubmed.ncbi.nlm.nih.gov/23531493/ - Persson LC, Carlsson CA, Carlsson JY. Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine (Phila Pa 1976). 1997 Apr 1;22(7):751-8. doi: 10.1097/00007632-199704010-00007. PMID: 9106315. https://pubmed.ncbi.nlm.nih.gov/9106315/
- Reddy PK, Sathyanarayana S, Nanda A. MRI-documented spontaneous regression of cervical disc herniation: a case report and review of the literature. J La State Med Soc. 2003 Mar-Apr;155(2):97-8. PMID: 12778993. https://pubmed.ncbi.nlm.nih.gov/12778993/
- Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine (Phila Pa 1976). 1996 Aug 15;21(16):1877-83. doi: 10.1097/00007632-199608150-00008. PMID: 8875719. https://pubmed.ncbi.nlm.nih.gov/8875719/
- Solomon J, Simotas A, Moley P, Lutz C. Aggressive nonoperative treatment for cervical radiculopathy due to HNP utilizing transforaminal cervical epidural injections: a prospective outcome study. Abstract presentation AAPMR 2004.
- Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014 Aug 1;14(8):1781-9. doi: 10.1016/j.spinee.2014.02.032. Epub 2014 Mar 12. PMID: 24614255. https://pubmed.ncbi.nlm.nih.gov/24614255/

