Knee Replacement

Summary: This article explains why knee replacement surgery os performed, how it works, and what patients can expect before, during, and after surgery. It reviews the difference between total and partial knee replacement, how the operations are performed, the materials used in knee implants, recovery and rehabilitation timelines, and how long results typically last.
Knee replacement is one of the most successful orthopedic surgeries performed today. Most patients experience reduced or eliminated knee pain, increased ability to move and an overall improvement in quality of life. HSS performs more total knee replacement surgeries than any other US hospital. HSS surgeons invented the first modern total knee replacement in the 1970s and have continually improved surgical techniques, technology and prosthetic materials ever since.
- What is knee replacement surgery?
- What are the different types?
- How is the surgery performed?
- What anesthesia is used?
- What are the implants made of?
- How do I avoid or postpone surgery?
- How do I know if I need surgery?
- Can it be an outpatient surgery?
- Can both knees be replaced?
- How long does the surgery take?
- What is the recovery time?
- How long does a knee replacement last?
- How successful is the surgery?
- Will my implant set off a metal detector?
- What can I expect at HSS?
- How to prepare for knee replacement
What is knee replacement surgery?
Knee replacement is where portions of the bones that form the knee joint are removed and replaced with artificial implants. It is performed primarily to relieve knee pain and stiffness caused by osteoarthritis.
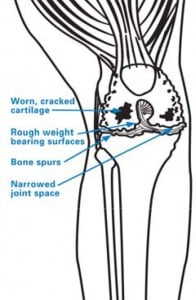
Most people who get this surgery have advanced knee arthritis, in which the knee cartilage is worn away and the surface of the knee becomes pitted, eroded, and uneven. This is sometimes referred to as “bone-on-bone" arthritis. This causes pain, stiffness, instability and a change in body alignment. Knee replacement surgery can also help some people who have a damaged knee joint caused by an injury or other condition.
Ask the Expert: Dr. Tony S. Shen explains total knee replacement
When arthritis wears down the cartilage in your knee, pain and limited mobility can make everyday life challenging. Tony S. Shen, MD, hip & knee surgeon at HSS, explains what knee replacement really does - who’s an ideal candidate, what to expect during surgery, and why choosing an experienced team matters for the best outcome.

An HSS Orthopedic Surgeon Explains Knee Replacement
What are the different types of knee replacement surgery?
There are two main types:
- total knee replacement, where the entire joint is replaced with artificial surfaces
- partial knee replacement, where only one damaged compartment of the knee is replaced
Total knee replacement is the more common of these two procedures.
Knee anatomy
To understand a total knee replacement, also known as total condylar knee arthroplasty, you must be familiar with the structure of the knee, a complex joint that consists of three bones:
- the femur (thighbone)
- the tibia (shinbone)
- the patella (kneecap)
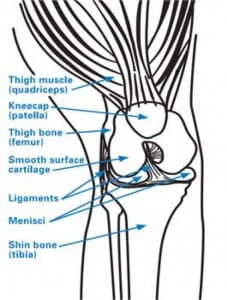
Strong ligaments connect the powerful muscles of the thigh and calf to the bones around the knee to control knee motion and function. Cartilage (such as the meniscus) and other soft tissues cover and cushion the bones to help them glide together smoothly.
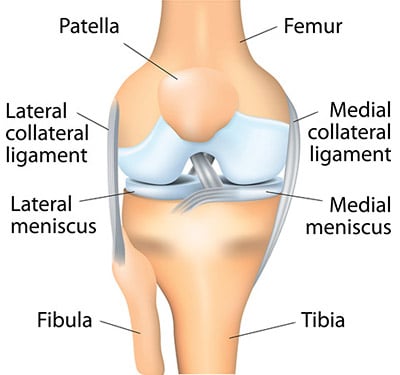
When you bend or straighten your knee, the end of the femur rolls against the end of the tibia, and the patella glides in front of the femur.
When the cartilage that cushions the joint degrades or is worn away completely, the bones rub together and become scraped and rough. This causes inflammation known as osteoarthritis, which results in pain and stiffness that make walking and other movement difficult. The implants used in knee replacement are smooth like the surfaces of a healthy knee.
How is a total knee replacement performed?
First, the orthopedic surgeon makes an incision (cut) in the knee and moves the patella (kneecap) to the side. If any bone spurs (small bony growths) are present, as sometimes occurs in osteoarthritis, they will be removed.
Next, the two menisci between the femur and tibia are removed, as are the anterior cruciate ligament (ACL) and, in some cases, the posterior cruciate ligament (PCL). In some types of knee replacement, the PCL is retained.
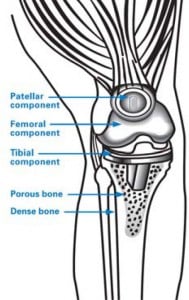
During the main phase of the operation, the surgeon cuts and removes cartilage and some bone from the upper part of the tibia and lower sections of the femur. The femoral sections removed are two knobby protuberances called the femoral condyles. The tibia and femur are then capped with metal implants to create new surfaces for the joint. The surface of the femoral component mimics the shape of the original femoral condyles. If the kneecap has also degraded, the surface on its underside may also be cut away and replaced with a polyethylene (plastic) implant.
Finally, the various layers of tissue are repaired with dissolvable sutures and the skin incision is closed with sutures or surgical staples. A bandage will be wrapped around the knee and the patient is taken to recovery.
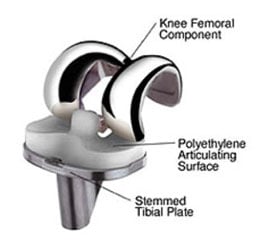
Fixed-bearing knee implant with a polyethylene articulating surface (plastic tray) sandwiched between the metal tibial implant and metal femoral implant.

Side-view illustration of a knee with a fixed-bearing knee implant in place.
In some cases, the orthopedic surgeon may employ computer navigation or robotic technologies during the operation.
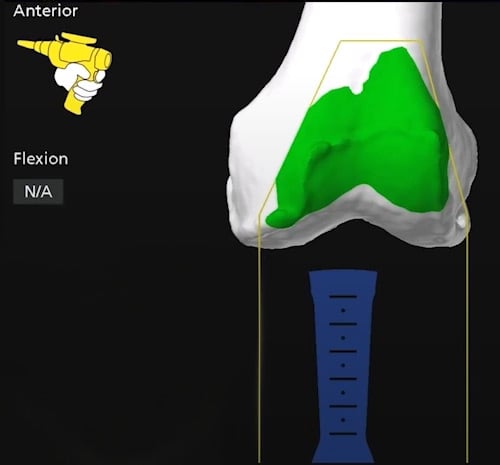
Real-time computer navigation image of a robotic arm used by an orthopedic surgeon on the front of the femur, prior to osteotomy.
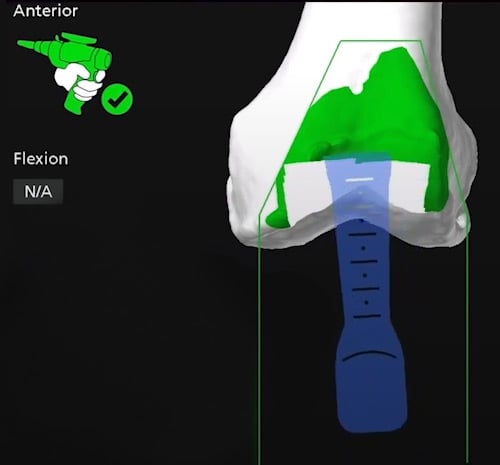
Real-time computer navigation image of the robotic arm at the start of the osteotomy to remove bone from the front of the femur.
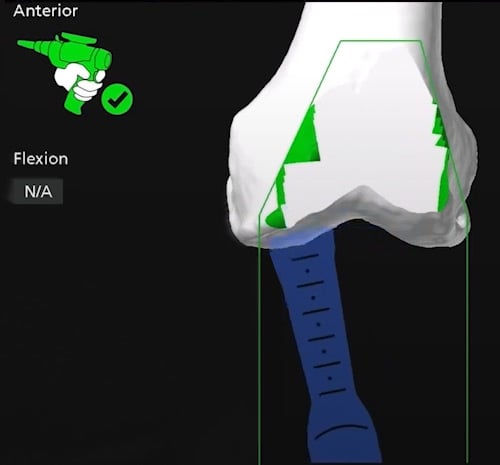
Real-time computer navigation image of the robotic arm near completion of the knee osteotomy to prepare the femur for an implant.
Video: Animation of a total knee replacement
What kind of anesthesia is used in a knee replacement?
Most total knee replacements at HSS are performed under regional anesthesia. It is called a spinal/epidural block, which is similar to the kind of anesthesia given to women in labor. The spinal/epidural anesthesia provides numbness from the waist down, so there will be no pain during surgery. In addition, patients are given a sedation to make them sleepy during the surgery. (Learn more by reading Anesthesia During Hip or Knee Replacement: What to Expect During and After Surgery.)
What are knee replacement implants made of?
The selection of knee replacement prosthesis design and materials depends on each individual patient. The main implant components are made of metal – usually titanium or chrome-cobalt alloys. The implants are fixated in place either with a cement bonding agent or by osseointegration, in which the patient’s bone grows into a porous metal surface. A plastic platform or spacer will be inserted between the tibial and femoral implant surfaces. The spacer is made of polyethylene.
Most femoral components are made of metal alloys (cobalt chromium) or metal-ceramic alloys (oxidized zirconium). The patellar component is plastic (polyethylene). The tibial insert component is also plastic (polyethylene). The tibial tray component can be made of the following materials:
- cobalt chromium (metal alloy)
- titanium (metal alloy)
- polyethylene (plastic)

Anteroposterior (front-to-back) X-ray of total knee replacement implants.

Lateral (side-view) X-ray of total knee replacement implants.
Partial knee replacement overview
A partial knee replacement is also known as unicompartmental knee arthroplasty or unicondylar knee arthroplasty. In this surgery, damaged cartilage and bone are removed and replaced only in one diseased compartment of the knee. This differs from a total knee replacement, in which bone and cartilage from the entire joint are replaced.
Partial knee replacement is suitable for people who experience arthritis only in one compartment (section) of the knee joint, rather than throughout the joint. It can also provide relief from pain and stiffness in some people who have medical conditions that make them poor candidates for total knee replacement surgery.
How do I avoid or postpone a knee replacement?
The choice on whether to have surgery to address arthritis of the knee joint depends on multiple factors, including:
- the condition of the knee joint
- the patient’s age and activity level
- the patient’s limitations due to their condition
In cases where the damage from arthritis is minimal, and/or if the patient does not have significant pain in the knee, nonsurgical treatments by be tried, including:
- physical therapy
- NSAIDs (nonsteroidal anti-inflammatory drugs), such as ibuprofen
- weight loss to reduce pressure on the knee and, in turn, slow down the advancement of arthritis
- One or more injection therapies, such as
- cortisone shots
- hyaluronic acid injections (viscosupplementation)
- experimental treatments such as stems cells or platelet-rich plasma (PRP)
For some patients, alternate, less invasive surgeries may delay the need for total knee replacement. This can include cartilage repair surgery, a knee osteotomy (such as a high tibial osteotomy) to realign the bone and reduce wear on the cartilage, or a partial knee replacement.
How do I know if I need knee replacement surgery?
You may need surgery if:
- Your knees are stiff and swollen.
- There is pain throughout the day, even at rest.
- Walking, getting up or climbing stairs is difficult and painful.
- Medication, injections and therapy do not offer enough relief.
- Knee cartilage is so damaged and worn away that you are walking "bone on bone," in which the bones of the joint are scraping together.
How long does a knee replacement last?
In most cases, an implant will last at least 20 years or longer. Younger patients who have a knee replacement and maintain an active lifestyle as they grow older may eventually require a knee revision surgery to replace the prosthesis.
Can knee replacement be done as an outpatient?
Some patients are able to return home the same day after an outpatient procedure, while others stay overnight in the hospital. (Learn more by reading Outpatient Knee Replacement Surgery: Frequently Asked Questions.)
Can both knees be replaced at the same time?
In most cases, it is safer to have one knee replacement performed, rather than both at the same time. Your orthopedist can tell you more about what is involved.
How long does knee replacement surgery take?
Total knee replacement surgery generally takes about 60 to 90 minutes, but you should expect to be in the operating room for over two hours.
How long does it take to walk after a full knee replacement?
Most often, within two or three days after surgery, a patient will be able to start walking with assistance from a straight cane, walker or crutches. The distance and frequency of walking will increase as the days progress.
Patients are usually able to drive a car within three to six weeks after surgery and resume most other normal activities by or before six weeks. Complete recuperation and return to full strength and mobility may take six months or more. However, in many cases, patients are significantly more mobile 1 to 2 months after surgery than they were before they had their knee replacement.
Knee replacement recovery time and recuperation
Rehabilitation (physical therapy) will begin within 24 hours of surgery. After your surgery, the nursing staff will position you in bed and help you turn until you are able to move on your own.
Very soon after surgery, a physical therapist will come to your room to teach you appropriate exercises and review your progress. Gentle exercises to improve your range of motion can help prevent circulation problems as well as strengthen your muscles.
Your rehabilitation program will begin as soon as you are medically stable and there are orders from your doctor to begin postoperative mobility. All patients begin rehabilitation within 24 hours of their surgery. Your motivation and participation in your physical therapy program is key to the success of your surgery and recovery. The physical therapist will assist you in the following activities:
- sitting at bedside with your feet on the floor
- transferring in and out of bed safely
- walking with the aid of a device (walker, cane, or crutches)
- climbing stairs with aid of a device
How successful is knee replacement surgery?
In general, total knee replacement is one of the most successful operations for improving pain and function in patients with end-stage osteoarthritis. Most patients experience significant pain relief and can return to many activities. It is important to talk to your surgeon about specific expectations regarding the recovery and outcome after knee replacement surgery. HSS Surgeons and engineers are continuously working to maximize effectiveness and satisfaction for all patients undergoing knee replacement surgery.
Will a knee replacement set off a metal detector?
While knee implants generally do not set off metal detectors, more sensitive machines may register the presence of the implant. It is not necessary to carry any sort of card or documentation for airport security.
What can I expect at HSS?
Hospital for Special Surgery has been at the forefront of modern knee replacement since the operation was first introduced in the late 1960s. We have led the field ever since in a number of ways:
- The numbers: HSS has been ranked the No. 1 hospital for orthopedics by U.S. News & World Report for 14 years in a row.
- Along with high rankings in patient satisfaction, HSS performs the most knee replacements with the lowest reported infection rates in the United States.
- Research and advancement: Smaller incisions, new implant materials and design, and sophisticated instrumentation have been – and continue to be – the areas of expertise of the hip and knee replacement surgeons of the HSS Adult Reconstruction & Joint Replacement Service.
- HSS routinely uses the latest surgical techniques and technology, such as robotic-assisted and computer-assisted surgery.
- Regional anesthesia: Isolating the anesthesia to a particular body area helps avoid the potential problems that may accompany a general anesthetic. These techniques have been developed and refined by the HSS Department of Anesthesiology, Critical Care & Pain Management.
How to prepare for knee replacement
There are certain steps that can improve your recovery time and results. It is important to follow your knee replacement surgeon’s instructions both before and after surgery, as well as that of your rehabilitation therapist’s recommendations.
Key takeaways
- Knee replacement involves replacing damaged portions of the knee joint with artificial implants to relieve pain and improve mobility.
- The procedure is most often used to treat severe arthritis, where cartilage is worn away and bone rubs against bone.
- Total knee replacement replaces the knee entire joint, while partial knee replacement replaces only one affected compartment.
- Most procedures use regional (spinal/epidural) anesthesia to minimize discomfort and aid recovery.
- Implants are made of metal alloys and polyethylene components, designed to replicate the smooth motion of a healthy knee.
- Computer- and robotic-assisted techniques help improve precision and outcomes.
- Recovery and rehabilitation begin within 24 hours of surgery; most patients walk with assistance in 2 to 3 days and resume daily activities within six weeks.
- Knee replacements typically last 20 years or longer. Knee revision surgery may eventually be needed for younger, active patients.
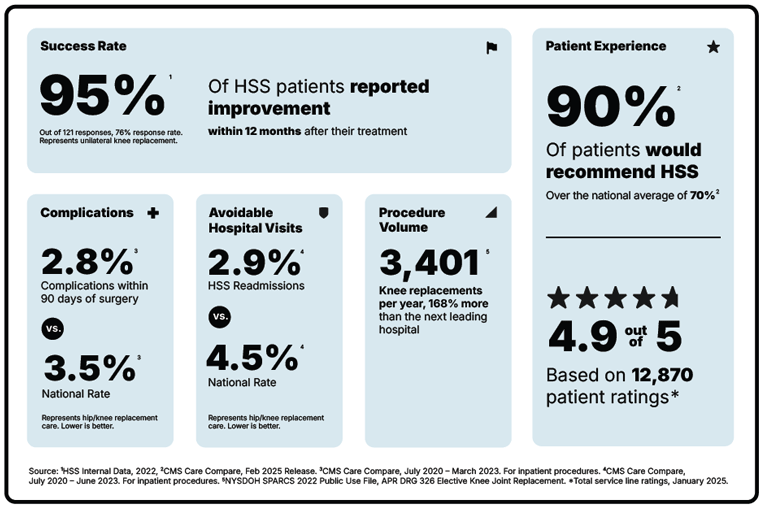
- HSS maintains the lowest infection rates in the nation and a 95% success rate, with 91% of patients recommending HSS for knee replacement.
- HSS’s multidisciplinary approach, which combines surgical expertise, research innovation, and specialized anesthesia, helps ensure the safest, most effective outcomes possible.
Why you should choose HSS for knee replacement
Knee replacement is a surgery focused on reducing pain and getting you back to the activities you love. But not all hospitals achieve the same results. Some are more reliable than others. With the help of the HSS Hospital Reliability Scorecard, you can make sure you're asking the critical questions to find the hospital that's right for you. Understanding the data points will help you make the best decision for your care. See hospital reliability data
Medically reviewed and updated by Cynthia A. Kahlenberg, MD, MPH, on behalf of the Adult Reconstruction and Joint Replacement Service
Knee Replacement Success Stories
References
- Beiene ZA, Tanghe KK, Kahlenberg CA, McLawhorn AS, MacLean CH, Gausden EB. Defining a successful total knee arthroplasty: a systematic review of metrics of clinically important changes. Arthroplasty. 2023 May 18;5(1):25. doi: 10.1186/s42836-023-00178-3. PMID: 37198708; PMCID: PMC10193600. https://pubmed.ncbi.nlm.nih.gov/37198708/
- Glenday JD, Vigdorchik JM, Sculco PK, Kahlenberg CA, Mayman DJ, Debbi EM, Lipman JD, Wright TM, González FJQ. A novel computational workflow to holistically assess total knee arthroplasty biomechanics identifies subject-specific effects of joint mechanics on implant fixation. J Biomech. 2024 Feb;164:111973. doi: 10.1016/j.jbiomech.2024.111973. Epub 2024 Feb 3. PMID: 38325192. https://pubmed.ncbi.nlm.nih.gov/38325192/
- Malkani AL, Roche MW, Kolisek FR, Gustke KA, Hozack WJ, Sodhi N, Acuña A, Vakharia R, Salem HS, Jaggard C, Smith L, Mont MA. New Technology for Total Knee Arthroplasty Provides Excellent Patient-Reported Outcomes: A Minimum Two-Year Analysis. Surg Technol Int. 2020 May 28;36:276-280. PMID: 31732961. https://pubmed.ncbi.nlm.nih.gov/31732961/
- Memtsoudis SG, Cozowicz C, Bekeris J, Bekere D, Liu J, Soffin EM, Mariano ER, Johnson RL, Go G, Hargett MJ, Lee BH, Wendel P, Brouillette M, Kim SJ, Baaklini L, Wetmore DS Hong G, Goto R, Jivanelli B, Athanassoglou V, Argyra E, Barrington MJ, Borgeat A, De Andres J, El-Boghdadly K, Elkassabany NM, Gautier P, Gerner P, Gonzalez Della Valle A, Goytizolo E, Guo Z, Hogg R, Kehlet H, Kessler P, Kopp S, Lavand'homme P, Macfarlane A, MacLean C, Mantilla C, McIsaac D, McLawhorn A, Neal JM, Parks M, Parvizi J, Peng P, Pichler L, Poeran J, Poultsides L, Schwenk ES, Sites BD, Stundner O, Sun EC, Viscusi E, Votta-Velis EG, Wu CL, YaDeau J, Sharrock NE. Peripheral nerve block anesthesia/analgesia for patients undergoing primary hip and knee arthroplasty: recommendations from the International Consensus on Anesthesia-Related Outcomes after Surgery (ICAROS) group based on a systematic review and meta-analysis of current literature. Reg Anesth Pain Med. 2021 Nov;46(11):971-985. doi: 10.1136/rapm-2021-102750. Epub 2021 Aug 25. PMID: 34433647. https://pubmed.ncbi.nlm.nih.gov/34433647/
- McCormick, John. "Augmented Reality Used in Knee-Replacement Surgery in a U.S. First," The Wall Street Journal, Jan. 21, 2021. https://www.wsj.com/articles/augmented-reality-used-in-knee-replacement-surgery-in-a-u-s-first-11611277959. Accessed Jun. 11, 2024.
- Ranawat AS, Ranawat C.S. (2012) The History of Total Knee Arthroplasty. In: Bonnin, M. (2012), The Knee Joint: Surgical Techniques and Strategies. Paris: Springer. https://doi.org/10.1007/978-2-287-99353-4_63.
- Sousa PL, Sculco PK, Mayman DJ, Jerabek SA, Ast MP, Chalmers BP. Robots in the Operating Room During Hip and Knee Arthroplasty. Curr Rev Musculoskelet Med. 2020 Jun;13(3):309-317. doi: 10.1007/s12178-020-09625-z. PMID: 32367430; PMCID: PMC7251009. https://pubmed.ncbi.nlm.nih.gov/32367430/