Contact Us!
Department of Biomechanics
AMT Center
510 East 73rd Street, Suite 202
New York, NY 10021
Anna Mirabal
Administrative Manager
TEL: 212.606.1754
Email: mirabala@hss.edu
Kate Meyers
Lab Manager
TEL: 212.606.1356
Email: meyersk@hss.edu
The mission of the Department of Biomechanics is to apply principles of engineering and materials science to solve orthopedic problems by conducting basic and applied research that translates to the development of orthopedic devices and instrumentation aimed at improved patient care. The Department also provides education and training for students pursuing careers in orthopedic surgery and biomedical engineering.
The Department’s research, development, and educational programs are conducted in collaboration with the Hospital’s Orthopedic Services, the Hospital’s Research Institute, and Cornell University, the latter through the Center for Advanced Materials and Engineering in Orthopaedics (CAMEO).
Specific areas of research include: the design and performance of total joint replacement systems including patient specific orthopedic devices; kinematics and contact mechanics of joints like the knee, ankle, and shoulder; biomaterials for joint restoration; and in vivo systems for measuring joint stability and mechanics.
A goal of the Department of Biomechanics is to provide training and education to clinical fellows in orthopedic biomechanics. This goal is achieved through a combination of didactic lectures embedded in clinical conferences, participation in case discussions, and providing fellows with opportunities to participate in specialty-specific research projects.
For some of the orthopedic services, such as Adult Reconstruction and Joint Replacement, the assignment of research projects is a formal process of the fellowship. However, any clinical fellow with an interesting research question or hypothesis that they have developed with a mentor from the surgical staff at HSS is welcome to present the topic to one of the weekly departmental meetings for constructive criticism and vetting.
The goal of the CAMEO program is to create a seamless partnership between Cornell Ithaca and HSS to enhance the cross-institutional application of engineering and materials science principles to musculoskeletal patient care. Members are required to be engaged (or planning to become engaged) in a research project that spans both institutions, includes both a clinician and engineer, and can be discussed at any annual retreat. Current foci for research under the CAMEO program include Translational Bone Mechanobiology, Arthritis and Joint Preservation, Functional Joint Arthroplasty, and Engineered Regenerative Medicine.
Students interested in participating in the CAMEO program as part of their undergraduate and graduate education should apply to Cornell University for admission and seek out Cornell faculty actively involved in the Program. Postgraduate students interested in fellowship opportunities should contact HSS or Cornell faculty actively involved in the Program.
Our NIH-funded Training Grant supports two 2nd year graduate students at Cornell University, Ithaca and two post-doctoral trainees (PhDs and MD Clinical Residents) at HSS providing them with unique training, mentoring, and research opportunities in interdisciplinary approaches to tackle orthopaedic clinical challenges. Trainees are jointly mentored by HSS and Cornell faculty. Interested applicants are encouraged to contact Dr. Suzanne Maher at HSS and Dr. Marjolein van der Muelen at Cornell. CAMEO opportunities for trainees.
In 2023 we were awarded two one-year Administrative Supplements to Recognize Excellence in Diversity, Equity, Inclusion, and Accessibility (DEIA) and to Better Incorporate Pain Related Research in Rheumatic, Skin and Musculoskeletal Diseases Workforce Development. Together these supplements support an additional 5 pre-doctoral trainees.
Hospital for Special Surgery offers clinical electives for students in their fourth year of medical school. Applications are accepted through the Visiting Student Learning Opportunities website, and applicants must meet all criteria to be accepted. Medical Student Elective placement runs on a first-come, first-served basis. However, Weill Cornell Medical College students are given priority via an open enrollment that precedes regular enrollment. Electives are offered from July through November to eligible students through AAMC Visiting Student Learning Opportunities® (VSLO®) program. Orthopaedic Biomechanics and Biomaterials Research is an elective with the Department of Biomechanics Chair as the primary mentor.
The Mary Rodgers and Henry Guettel Fellowship in Biomedical Mechanics is a postgraduate fellowship utilizing the resources of HSS and the Section of Biomechanics of the Sibley School of Mechanical and Aerospace Engineering, Cornell University. The focus of the fellowship is to develop expertise in Biomedical Mechanics and Materials specifically as it relates to orthopedic biomechanics. The selected fellow is mentored by surgical and biomechanics staff from HSS as well as the biomedical engineers working within the CAMEO Program.
HSS has a longstanding collaboration with the United States Military Academy at West Point through clinical collaborations in research and fellowship training for West Point surgeons in the Hospital’s Sports Medicine service.
In recent years, the collaboration has been extended to hosting USMA cadets interested in biomedical engineering or medical careers in the Department of Biomechanics. Immersing the cadets into the Department for a month, they experience a broad array of ongoing orthopedic research projects with the opportunity to participate in data collection and analysis and in laboratory meetings and clinical conferences. The goal is to provide the cadets with a firsthand understanding of how multidisciplinary translational research can address clinically relevant questions with the goal of improving patient care.
Each year members of our department volunteer to participate in the Perry Initiative. This is a one-day program, championed by Dr. Shevaun Doyle, for young women in high school to explore careers in orthopedic surgery, engineering, or both. In this workshop, students have the opportunity to learn about various aspects of orthopedics and biomechanics through lectures, hands-on activities, and question and answer sessions. Engineers, Residents, Clinical and Research Fellows, and Attending Surgeons work together to give an overview of these exciting career options.
1985: Dr. Wright collaborates with Dr. Eduardo Salvati, Dr. Barry Brause, and Dr. John Callaghan, a clinical fellow to win the Frank Stinchfield Award from the Hip Society for research into the biomechanical, pharmacokinetic, and clinical impacts of antibiotic additions to bone cement for the treatment of periprosthetic joint infection in total hip arthroplasty.
1989: Dr. Burstein is awarded the Alfred R. Shands, Jr., MD Award given by the Orthopaedic Research Society in recognition of the devotion of a significant portion of a professional lifetime to furthering knowledge in the fields of musculoskeletal disease.
1989: Drs. Bartel, Rimnac, and Wright win a Kappa Delta Award from the American Academy of Orthopaedic Surgeons, the top prize in musculoskeletal research, for their research elucidating the mechanics of oxidation and wear in polyethylene joint replacement components.
1992: Dr. Wright serves as President of the Orthopaedic Research Society. Preceded by Dr. Philip D. Wilson, Sr (1956) and Dr. Joe Lane (1984) and followed by Dr. Adele Boskey (1996), Dr. Mary Goldring (2014), Dr. Mathias Bostrom (2015), Dr. Marjolein van der Meulen (2022), and Dr. Suzanne Maher (2024), Dr. Wright joins the longest list of Presidents from one institution in the history of the ORS.
1994: Drs. Rimnac and Wright collaborate with surgeon Mathias Bostrom, MD, to win the Mark Coventry Award from the Knee Society for their research describing the natural history of polyethylene degradation in knee replacement components from the time of manufacturing to implantation.
1997: Dr. Wright receives a Director's Special Citation from the U.S. Food and Drug Administration for his work on a forum of academic, industry, and FDA representatives striving to improve the regulatory process for orthopedic devices.
2011: Dr. Don Bartel becomes the second member of the Department (after Dr. Burstein in 1989) to receive the Alfred R. Shands, Jr., MD Award from the Orthopaedic Research Society for a professional lifetime of significant contributions to musculoskeletal research.
2011: Asheesh Bedi, MD, Mark Dolan, MD, Iftach Hetsroni, MD, Erin Magennis, MSc, Joseph Lipman, MS, Robert Buly, MD, and Bryan T. Kelly, MD., won this year's AOSSM Excellence in Research Award for their presentation titled, “Surgical Treatment of Femoroacetabular Impingement Improves Hip Kinematics: A Computer Assisted Model.”
2013: Dr. Wright becomes the third member of the Department (after Dr. Burstein in 1989 and Dr. Bartel in 2011) to receive the Alfred R. Shands, Jr., MD Award from the Orthopaedic Research Society for a professional lifetime of significant contributions to musculoskeletal research. Three is the greatest number of Shands Awards made to individual members of the same research laboratory in the more than 50-year history of the Award.
2015: George Triantafyllopoulos, MD, a clinical fellow, and his colleagues Dr. Wright, Dr. Christina Esposito, Dr. Doug Padgett, Dr. Jayme Burkett, and Marci Elpers win the Otto Aufranc Award from the Hip Society for their research showing that head size does not affect fretting and corrosion damage at the head-neck taper of metal-on-polyethylene total hip arthroplasties.
2020: Dr. Burstein, now Emeritus Senior Scientist at HSS, is presented with the Lifetime Achievement Award by the Knee Society for his contributions to education, research, and development efforts centered on knee replacement surgery.
2020: Joey Romero, MD, a clinical fellow, and his colleagues Dr. Wright, Dr. Padgett, Dr. Geoffrey Westrich, Amanda Wach, Scott Silverberg, and Yu-Fen Chiu win the Otto Aufranc Award for outstanding research from the Hip Society for work examining the clinical and tribocorrosion aspects of malseating in modular dual-mobility liners.
2020: Niv Marom, MD, and his colleagues Hervé Ouanezar, Hamidreza Jahandar, Zaid Zayyad, Thomas Fraychineaud, Daniel Hurwit, Carl Imhauser, Thomas Wickiewicz, Andrew Pearle, and Danyal Nawabi are awarded the Cabaud Memorial Award from the American Orthopaedic Society for Sports Medicine for their work showing that lateral extra-articular tenodesis reduces anterior cruciate ligament graft force and anterior tibial translation in response to applied pivoting and anterior drawer loads.
2020: Dr. Glenday, a postdoctoral fellow, and his colleagues Quevedo Gonzalez, Wright, Lipman, Sculco, and Vigdorchik receive the best presentation award at the New Early-Career Webinar Series of the International Society for Technology in Arthroplasty for their work evaluating the effect of varus alignment on the bone-implant interaction of cementless tibial baseplates
2022: Dr. Brett Steineman and colleagues win the J. Leonard Goldner Award for Outstanding Basic Science Paper at the Annual Meeting for the American Orthopaedic Foot & Ankle Society for a manuscript describing a study of passive eversion assessment for progressive collapsing foot deformity after lateral column lengthening.
2023: Dr. Steineman receives a New Investigator Recognition Award from the Orthopaedic Research Society for his research on a statistically augmented computational approach using geometric MRI-derived biomarkers as predictors of changes in joint mechanics after partial meniscectomy.
2023: Dr. Wright receives the Lifetime Achievement Award from the International Society for Technology in Arthroplasty.
In the 1960’s and early 1970’s, HSS surgeons began exploring existing methods for restoring joints with metal and plastic parts. Realizing that existing solutions were unsatisfactory, they began exploring new designs and innovative surgical techniques for advancing joint replacement. The reimagining of the Biomechanics Department in later that decade set the stage for the advent of the first modern knee replacement that not only eliminated crippling joint pain, but also provided functionality and durability.

HSS Surgeon-in-Chief Philip D. Wilson, Jr., MD, recruits Al Burstein, PhD, to lead the newly formed Department of Biomechanics in the same year that Congress passes the first Medical Device Regulation Act. Drs. Wilson and Burstein conceive of a team that can collaborate with surgeons on device design and development, including the regulatory pathway for medical devices through the FDA, but can also lead the way in patient-specific implants.
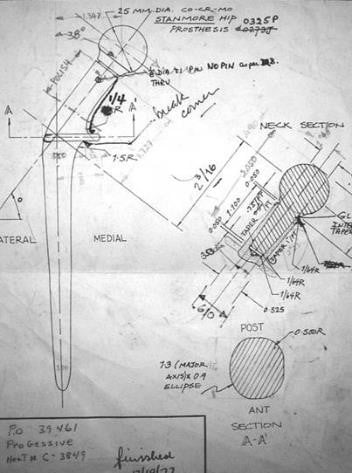
The first-ever patient-specific implant, a hip, is designed by Dr. Burstein in collaboration with Dr. Wilson, Jr, the prescribing physician. Its successful implantation solidifies the pivotal role of bioengineers in helping to solve complex orthopedic problems.
The department establishes a postdoctoral fellowship in biomechanics, with Tim Wright, PhD, as its first fellow. The program will go on to distinguish itself as a training ground for adding some of the field's most innovative biomechanical engineers to the staff, including Dr. Wright; Suzanne Maher, PhD; Carl Imhauser, PhD; Tony Chen, PhD; Fernando Quevedo Gonzalez, PhD; Brett Steineman, PhD; and Aarti Shenoy, PhD.

A newly initiated implant retrieval system at HSS sets the stage for a thriving program of R&D. The system offers a method by which all implants removed from patients during surgery are tracked from the operating room to pathology to biomechanics, where they are then cleaned, boxed, and stored for future analysis. Today, nearly 30,000 implants have been retrieved.
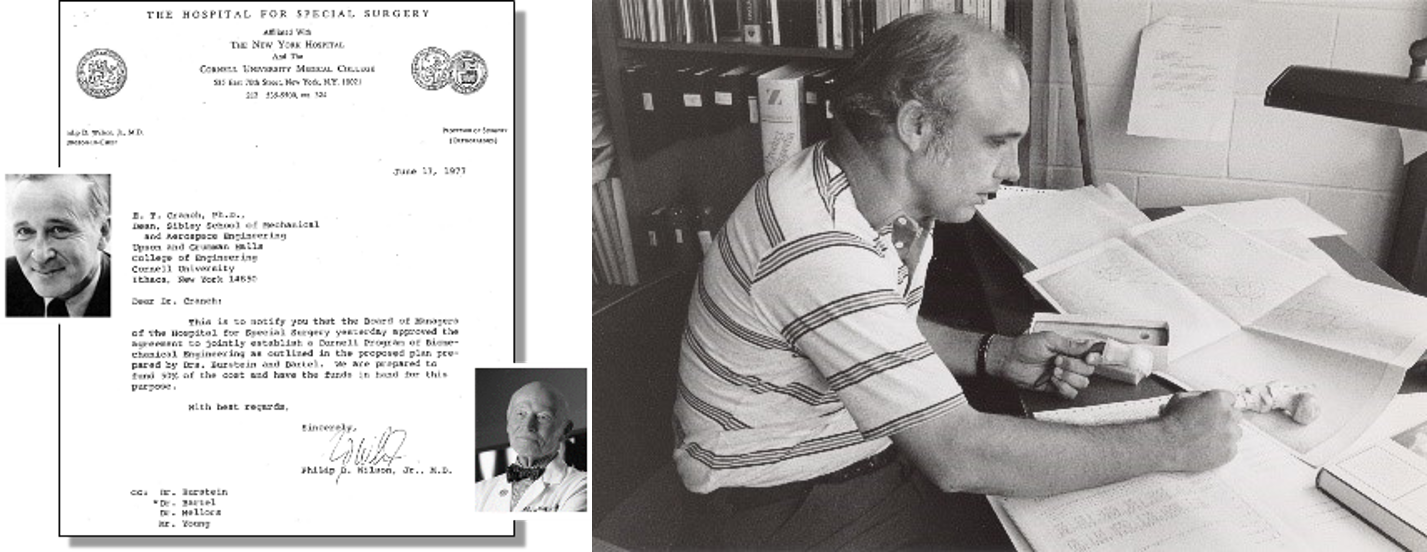
HSS deepens its research ties with Cornell University, creating the Cornell-HSS Program in Biomechanical Engineering. The one-of-a-kind training program for Cornell master's and doctoral students emphasizes translational and applied research into clinical problems through direct encounters with orthopedic surgeons in the OR and other clinical settings.
Jim Otis, PhD, from the Biomechanics Department, and Leon Root, MD, develop the first gait analysis capabilities at HSS within the rehabilitation department. The effort expands into the current Leon Root, MD, Motion Analysis Laboratory for the collection, analysis, and interpretation of human movement data.
Dr. Burstein and John Insall, MD, develop and patent concepts for the first posterior-stabilized knee replacement. The device has a significant, immediate impact on patients' quality of life, as patients can easily climb stairs and get in and out of a chair without assistance — tasks that were difficult to impossible with predecessor devices. The device finds large-scale clinical and commercial success.

Computational power begins to transform the field, evolving implant design and taking the process from pen and paper to CAD/CAM. Fundamental insights into polyethylene components set the stage for an accelerated program of materials research in the 1990s.
A second-generation posterior-stabilized knee comes to fruition when Drs. Insall and Burstein join forces with Don Bartel, PhD, of Cornell University. The introduction of computer modeling as well as advancements in radiographic imaging and retrieval analyses enable enhanced designs that afford improved wear resistance and provide greater range of motion and improved stability.
Dr. Wright and colleagues show that antibiotics can be added to bone cement at the time of surgery to help eradicate infection without adversely affecting fixation of the implant. This multidisciplinary research that integrates engineering with orthopaedic surgery and infectious diseases, assured commercial interests that they could commercially introduce cements with prepackaged antibiotics.

A new, state-of-the-art orthopedic implant facility, funded by a grant from the Dana Foundation, opens on 73rd Street in Manhattan. The Dana Center, as it will be known until 2021, represents the shift from manual machining of patient-specific implants to the computer-assisted design and manufacturing of entire knee and hip implant systems to supply the operating rooms at HSS.
Research by Drs. Bartel, Rimnac, and Wright elucidates the mechanics of oxidation and wear in polyethylene joint replacement components. The work results in a Kappa Delta Award, the top prize in musculoskeletal research.
Research and development lead to further perfection of total knee replacement. Tim Wright takes the reigns of the department. New avenues of biomechanics research open up in areas such as mechanobiology further enhancing collaboration between HSS and Cornell bioengineers.
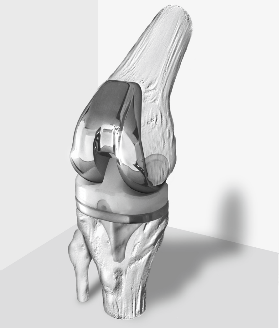
HSS introduces its fourth-generation total knee replacement device, called Optetrak. The new system takes the team one step closer to achieving uniformly optimal results, lowering the wear rate by reducing polyethylene stresses, eliminating patellar problems through tracking improvements, and providing greater than 120° range of motion.
Dr. Wright is named Director of the Biomechanics Department at HSS, while also stepping into the role of President of the Orthopaedic Research Society. The Society has existed as the leading international forum for musculoskeletal research. During that time, six members of the HSS staff have served as President, more than any other institution in the Society’s history.
Steve Li, PhD, advances the department's ongoing research into polyethylene degradation and develops intellectual property aimed at improving wear resistance through pressure/thermal treatments.
Drs. Rimnac and Wright collaborate with surgeon Mathias Bostrom, MD, to elucidate the natural history of polyethylene degradation in knee replacement components, from the time of manufacturing to implantation. This research was only possible at HSS, an institution that manufactured implants from raw polyethylene materials, implanted the devices into patients, and then recovered retrieved implants that had failed so that the degradation process could be studied from beginning to end. The work results in a Knee Society Award.

The department begins to diversify its research focus with the joint recruitment with Cornell University of Marjolein van der Meulen, PhD, and later Betsy Myers, PhD, in 1999. Their collaborations lead to the development of a large program studying biomechanical and biological adaptation of bone in response to disease, trauma, and treatment.
Dr. Wright receives an NIH P30 grant to establish the Center for Musculoskeletal Integrity at HSS, one of only two original centers for musculoskeletal research in the nation. The grant results in the formation of three new multidisciplinary cores in Analytical Microscopy, Infrared Imaging, and Mechanical Testing.
The emphasis on the biological side of the bone-implant system continues with the emphasis on further improving the longevity of joint replacements. Simultaneously, the Department’s research efforts extend into joint restoration, applying the principles in hip and knee joint replacement maintaining healthy cartilage and to reconstructing damaged ligaments.

Joe Lipman is named as Director of Device Development, expanding the design capabilities in the Department and facilitating improved collaboration with engineering staff on developing implant systems and on designing devices for specific patients with complex needs.

The recruitment of Suzanne Maher, PhD, reflects a burgeoning interest in applying insights from joint replacement design to joint restoration. After a post-doctoral fellowship in the intramural program at NIH, Suzanne starts to build models for the pre-clinical testing of scaffolds for joint repair.
The Optetrak Logic knee, the next generation of knee design, is developed by Drs. Bartel and Wright, Joe Lipman and surgeon collaborators Thomas Sculco, MD, and Geoffrey Westrich, MD. The design incorporates modifications to the anterior surfaces of the posterior stabilizing mechanism, while also providing an efficient, bone-preserving surgical technique and improved kinematics.

Carl Imhauser, PhD, joins HSS, initiating a program of research focused on the computational modeling of joint movement and function. This effort will go on to revolutionize research into joint kinematics, setting the stage for using models to develop precision surgery aimed at an individual patient’s need based on their anatomy and function.
Insights into cartilage repair result in the first spin-off technology to come out of HSS. Lessons learned in the hip and knee are applied to other joints like the ankle and elbow. And the team tackles a series of problems related to corrosion of modular hip components and the resulting catastrophic tissue destruction. Team-based science blossoms as researchers, clinicians and other scientists reach out to the Biomechanics Department to tackle multi-disciplinary problems.
The Adult Reconstruction and Joint Replacement Service and the Biomechanics Department organize the first combined Chinese Orthopaedic Association-HSS Symposium on Total Knee Arthroplasty at the COA meeting in Beijing. The symposium sets the stage for educational and collaborative efforts that have continued to develop between HSS and leading academic and clinical centers in China.
Dr. Maher and Russell Warren, MD, establish AGelity Biomechanics, a medical device company with the imperative to develop a mechanical solution for articular cartilage damage. It is the first spin-off technology from HSS. The company will go on to receive a BioAccelerate NYC Prize, a citywide competition to provide funding for biomedical research with significant commercial promise. The company will also receive both Phase I and Phase II funding from the NIH Small Business Innovation Research (SBIR) program.
The AIM Laboratory for Foot and Ankle Research is established with the help of Jonathan Deland, MD, and a grateful benefactor. The laboratory is centered around a “six degrees of freedom” robotic platform that moves a force plate about the tibia while linear actuators apply prescribed loading profiles to the tendons of the foot and ankle. The robot can simulate activities like walking and stair climbing.
George Triantafyllopoulos, MD, and his colleagues win the Otto Aufranc Award from the Hip Society for his research showing that head size does not affect fretting and corrosion damage at the head-neck taper of metal-on-polyethylene total hip arthroplasties.
An immersion term is initiated for engineering students from the United States Military Academy at West Point. Developed by Drs. Maher and Wright in collaboration with Lt. Col. Matthew Posner, MD, the summer term allows two cadets to spend a month in the department’s laboratories gaining firsthand experience in musculoskeletal research. He becomes the principal investigator on the NIH-funded SBIR phase I & II grants awarded to AGelity Biomechanics.

Tony Chen, PhD, joins the HSS faculty to study changes in joint contact mechanics after injuries and the ability of repair technologies in restoring normal joint loads. He becomes principal investigator on the NIH-funded SBIR phase I & II grants awarded to AGelity Biomechanics.
A celebration is held on the 40th anniversary of the original Cornell-HSS Program, with alumni and important guests from both institutions in attendance. The celebration includes a planning session for revitalizing the program as CAMEO, the Center for Advanced Materials and Engineering in Orthopedics.

Dr. Fernando Quevedo Gonzalez joins the Biomechanics faculty after a successful post-doctoral fellowship at HSS. Dr. Quevedo Gonzalez brings unique talents in computational modeling and optimization, techniques that he has applied to the design of cementless implant components for the knee, thumb, and ankle.
Joey Romero, MD, and his colleagues win the Otto Aufranc Award for outstanding research from the Hip Society for work examining the clinical and tribocorrosion aspects of malseating in modular dual-mobility liners.
Niv Marom, MD, is awarded the 2020 Cabaud Memorial Award from the American Orthopaedic Society for Sports Medicine for his work showing that lateral extra-articular tenodesis reduces anterior cruciate ligament graft force and anterior tibial translation in response to applied pivoting and anterior drawer loads.

Brett Steineman, PhD, joins the faculty of the department, specializing in combining dynamic cadaveric experimentation with computational models to address clinically relevant questions associated with total ankle arthroplasty, progressive collapsing foot deformity, and other challenges related to the lower extremities.
HSS partners with Italian device manufacturer LimaCorporate to open the first on-site additive manufacturing 3D printing facility. This collaboration sets the stage to substantially increase the availability and speed of personalized orthopedic care for patients with complex orthopedic conditions in the United States.

Aarti Shenoy, PhD, joins HSS after a postdoctoral fellowship exploring tribocorrosion at modular connections between joint replacement components. She applies her expertise in materials science to broaden studies of implant performance utilizing the implant retrieval program.
The Department’s future is focused on integrating the research and development efforts that have been the keys to its success over the past four decades. Combining emerging technologies like 3D printing, computational modeling, and advances biomaterials will provide revolutionary advancements in the development and patient-specific application of precision surgical solutions to patients suffering from joint problems. Adding to this approach continuing advancements in imaging, immunology, surgery, and genetics will allow multidisciplinary, team-science efforts to provide holistic advancements in musculoskeletal care.
The success of the Department of Biomechanics depends solely on the insightful clinical observations, intriguing clinically important questions, and the novel innovative ideas that stem from our “Surgeon Champions.” The collaboration between the Orthopedic Services and the Biomechanics Department staff provides a rich collegial environment from which to pursue research, product development, and educational initiatives.





Department of Biomechanics
AMT Center
510 East 73rd Street, Suite 202
New York, NY 10021
Anna Mirabal
Administrative Manager
TEL: 212.606.1754
Email: mirabala@hss.edu
Kate Meyers
Lab Manager
TEL: 212.606.1356
Email: meyersk@hss.edu