Surgery for People With Inflammatory Arthritis
The success of any surgical procedure is dependent upon a multitude of factors including the patient's overall health, their ability to adhere to a physical therapy regimen and the surgeon's skill, to name just a few.

But for patients with inflammatory arthritis, a range of systemic diseases involving the immune system, surgery involves a particularly complex set of considerations that arise from both the illness itself and the medications used to treat it.
In patients with inflammatory arthritis the immune system "perceives" the cartilage of the joint as foreign substance. The synovium, a layer of tissue that lines the joint and provides a lubricating fluid that also delivers nutrients to the cartilage, becomes aggravated and overgrows. An inflammatory response follows and the cartilage erodes, causing pain, stiffness, and eventually destruction of the joint, to the point where the bone rubs against bone. (This last stage of the disease process is similar to that seen with osteoarthritis, which occurs far more commonly and is not a systemic disease; other factors cause damage to the joint.) Conditions that fall into the category of inflammatory arthritis include:
In recent years, medical treatments for these conditions have expanded considerably. Drugs that reduce inflammation, those that suppress the immune response, and a group of biologic agents called DMARDs (disease-modifying anti-rheumatic drugs), have helped many patients with inflammatory arthritis control their symptoms and eliminated or delayed the need for surgery on joints damaged by disease.
Fortunately, due to the improvements in medical treatment, it is uncommon for a person to have inflammatory arthritis that significantly affects multiple joints. More commonly, people will have monoarticular or pauciarticular disease, meaning it involves one to three joints. These patients tend to be older and more active when they become candidates for joint replacement surgery.
A team approach for the surgical patient
To deal with the complexities of treating those patients with inflammatory arthritis who do require orthopedic surgery, at Hospital for Special Surgery (HSS), a collaborative approach is used. Orthopedic surgeons work closely with a team that includes a rheumatologist (the physician who oversees the non-surgical treatment of the disease), an anesthesiologist, a physical therapist, a social worker, and in some cases, psychologists or psychiatrists, and a biomechanical engineer. In addition to the systemic nature of the disease, and the effect of medications, this group must consider:
- the effect the disease can have on multiple joints
- physical limitations
- psychosocial challenges
- complex deformities
- poor bone quality
- higher complication rates

This picture demonstrates severe and advanced RA in which significant joint damage has occurred.
"Because some medications suppress the ability to fight infection following surgery, it's important that the orthopedist and rheumatologist determine the best way to protect the patient," explains Mark P. Figgie, MD, Chief Emeritus of the Surgical Arthritis Service. "That might include temporarily stopping medication or scheduling surgery during an interval between doses of medication." However, stopping immunosuppressive medications also carries a degree of risk since it may result in a flare-up of arthritis during recovery from surgery. As a result, the patient may be unable to follow a rehabilitative physical therapy program. Moreover, says Dr. Figgie, temporarily stopping medication can be problematic since in some instances, they are not as effective once they are resumed.
Compounding the difficulty of the treatment of inflammatory arthritis is the disease's effect on multiple joints at the same time. Rheumatoid arthritis, for example, is often bilateral, that is, both hips, or knees, or elbows, are affected. In cases where a series of surgeries are required, the orthopedic surgeon must determine the optimal order of these operations to achieve the best possible results.
"Usually we try to address the most painful area first," explains Dr. Figgie. "However, we also follow certain guidelines based on experience." In most cases, if the patient is having problems in the shoulder, elbow, hand and wrist, Dr. Figgie treats the wrist before the hand, since surgery on the wrist may affect the length of bones and tendons, which in turn will affect the function of the fingers. After the hand and wrist have been treated, the surgeon addresses the elbow, since a pain-free, stable elbow is critical to performing most activities of daily living. Shoulder surgery may also offer functional improvement, but often not to the same degree as with the elbow. A similar rationale is used for problems of the leg, usually treating the ankle and foot first, then the hip, and finally the knee.
"Given equal pain and disease involvement, you usually want to establish a pain-free, well aligned foot and ankle," says Dr. Figgie. "If the foot is deformed or painful, it will affect the patient's ability to function after knee and hip surgery. We usually address the hip before the knee because hip pain will radiate to the knee, and it is tough to rehabilitate the knee if the hip is stiff and painful."
Once a treatment plan is developed, physical therapists and social workers also play a key role in the process since they are often in the best position to evaluate the patient's special needs, capabilities and limitations in everyday life. Prior to surgery, the therapist can perform a functional evaluation of the patient to help determine if the planned surgery will offer the desired benefit. For example, depending on the joint in question and the patient's other disabilities, a fusion (a procedure that stiffens a joint) that might relieve pain might restrict the patient's ability to care for her or himself.
Therapists also help plan what the patient will need after surgery, including equipment such as walkers or canes, which may have to be customized to accommodate other joint involvement. In the treatment of juvenile arthritis, the therapist makes sure that rehabilitative equipment is the right size. Assessment of the home environment and the patients' support system are also important factors in predicting the success of surgery. Because some patients with inflammatory arthritis cannot tolerate traditional general anesthesia due to deformities or instability of the spine, the anesthesiologist must be skilled in administering regional anesthesia. Other patients may require fiberoptic intubation (a process in which a fiberoptic scope is used to ensure that the tube that delivers anesthesia is properly placed.)
"At HSS, we have an outstanding anesthesia department. It is the finest I have ever worked with," says Dr. Figgie. "We are able to perform close to 100% of our joint replacements under regional anesthesia. Not only is it safer, but the patients have better pain control postoperatively, and therefore recover faster."
Engineers in the hospital's Department of Biomechanics may also become part of the process. In cases where the patient requires a joint replacement, deformities caused by the disease may dictate the need for a custom-made prosthesis. This is especially true in patients with juvenile inflammatory arthritis, where the early onset of the disease will affect the size and shape of the bone. An HSS engineer designs the prosthesis, along with the surgeon, and the implant is then manufactured by one of the implant companies.
Finally, a psychiatrist or psychologist may be called upon to help patients cope with the demoralizing effect that both the disease, and the need for repeat surgeries and hospitalizations, may have.
Types of surgery for inflammatory arthritis
Surgical options for inflammatory arthritis include synovectomy, joint replacement (arthroplasty), and joint fusion (arthrodesis). The choice of surgery is made on an individual basis and takes into account the patient's age, obtaining the most predictable results, achieving the greatest pain relief, and preserving the maximum degree of function and independence. In addition, surgeons strive to select the procedure that will be the most durable. When the patient needs multiple surgeries, Dr. Figgie and his colleagues try to do as much as possible during a single hospitalization, a strategy that not only reduces the length of recovery, but also offers a psychological benefit.
"We try to combine procedures as much as possible in order to reduce hospitalization, rehabilitation and anesthesia. It really helps the patient cope better with the disease when we are able to do that," says Dr. Figgie.
Synovectomy
In inflammatory arthritis, the synovium grows abnormally and produces an excessive amount of fluid that "eats away" at the cartilage, which results in pain and swelling. With a synovectomy, the orthopedic surgeon removes most of the synovium, and the process is arrested. Results can be dramatic, but over a period of several years, the tissue grows back and the patient's symptoms may return. Synovectomy is an option only in patients with intact cartilage, usually in early stages of the disease, and may be done either as an open procedure or with arthroscopy (an operative technique in which a few small incisions are made and the surgeon uses fiberoptic technology and small instruments to perform the surgery.)
Open synovectomy vs. arthroscopic synovectomy
Open surgery offers greater access to the joint and allows the surgeon to remove more of the synovium during the operation, however, it requires cutting through muscle, resulting in greater discomfort to the patient, and a longer recovery period. Arthroscopic synovectomy is easier on the patient, but the problem may recur sooner if the removal of synovium is not as complete. However, it is less traumatic for the patient to undergo repeat arthroscopic surgery than to do repeated open procedures. After surgery, the patient continues to take his or her medication to delay recurrence in the treated joint and to protect other joints. The dose of medication may be reduced after successful synovectomy.
Joint replacement (arthroplasty) for inflammatory athritis
When the cartilage in a joint is severely damaged, replacement with a prosthesis may be necessary. Hip, knee, shoulder, and elbow replacements are done frequently, often with good results. Replacement of the ankle, wrist, and fingers are less commonly attempted, and yield less predictable results. Unlike synovectomy, arthroplasty usually offers a lasting solution to the problem of synovial inflammation and joint destruction, and provides significant pain relief. Once the articular surface is replaced, the symptoms are relieved.

Post-op X-ray of patient who has undergone arthroplasty of both hips.

Post-op X-ray of patient who has undergone arthroplasty of both knees.
Most patients need to continue taking medication to protect their other joints. In some cases, however, if the most problematic joint is treated successfully, the dose of medication taken may be reduced. "That offers a real benefit," Dr. Figgie says. "Many of these medications take their toll on the patient. Steroids can cause bone and muscle atrophy, and there's the ongoing problem of suppressing the immune system."
Joint fusion (arthrodesis)
In arthrodesis, the affected joint is fused, eliminating both motion and discomfort. This surgery is considered a "last resort" treatment since the associated lack of mobility can hinder the patient's functional ability. In certain joints, however, where range of motion is less important as in the heel or in the big toe, this surgery can provide a satisfactory and lasting resolution of symptoms. As with arthroplasty and synovectomy, the patient continues to take medication to protect their other joints, although the dosage may be reduced.
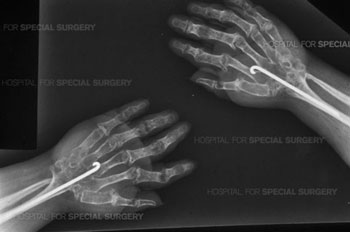
Post-op X-ray of patient who has undergone arthrodesis of both wrists.
"In most situations, we try to preserve joint motion, in order to reduce demands on the other joints. However, in some situations, an arthrodesis is the best option," says Dr. Figgie.
Potential surgical complications
Patients with inflammatory arthritis are at greater risk for complications associated with surgery than individuals without the disease. In addition to lowered immunity due to drug therapy, the quality of their bones, and deformities of the joint may contribute to poor outcome. Some problems are diagnosis-specific. Patients with lupus, for example, are particularly vulnerable to avascular necrosis (AVN), also known as osteonecrosis, a condition in which blood supply to the bone is cut off and the bone dies. This may occur due to the high doses of steroids that are required to control their disease. Patients with Ankylosing Spondylitis have more difficulty regaining motion due to the stiffness of their tissues from the disease.
The orthopedists and rheumatologists who serve on the Surgical Arthritis Service at HSS have many years of experience in treating patients with inflammatory arthritis. Indeed, many patients have formed close relationships with this group of physicians and their colleagues who continue to treat each stage and development of the disease.
Updated: 4/27/2022
Authors
Chief Emeritus, Surgical Arthritis Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery


