Posterior Tibial Tendon Dysfunction
- What is posterior tibial tendon dysfunction?
- What are the symptoms of posterior tibial tendon insufficiency?
- What causes posterior tibial tendon insufficiency?
- What are the stages of posterior tibial tendon insufficiency?
- How is posterior tibial tendon insufficiency treated?
What is posterior tibial tendon dysfunction?
Posterior tibial tendon dysfunction (also called posterior tibial tendon insufficiency or adult acquired flatfoot) literally means the failure of the posterior tibial tendon. However, this condition also involves the failure of associated ligaments and joints on the medial (inner) side of the foot and ankle. This results in collapse of the arch of the foot (commonly called "flatfoot" or "flat foot"), along with foot and sometimes ankle deformities that can become debilitating or disabling in later stages.
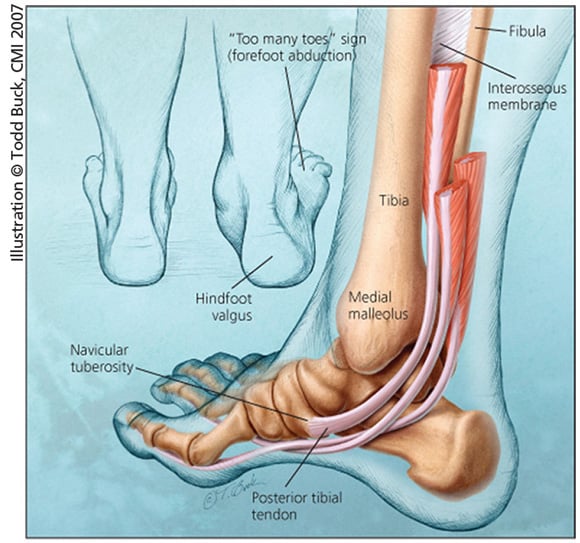
Figure 1: Anatomical diagram of the foot and ankle highlighting effects of posterior tibial tendon insufficiency.
[Illustration courtesy of the Journal of Musculoskeletal Medicine]
What are the symptoms of posterior tibial tendon dysfunction?
- Pain over the tendon in the inner part of your hindfoot (rear portion of your foot) and midfoot is the first common symptom.
- A deformity in the foot may develop, and this can make it difficult for you to walk. A common deformity is for the foot to sag downward and inward toward the opposite foot.
- As the tendon degenerates and loses its function, ligaments on the same inner side of the foot will also deteriorate and fail. Ligaments are soft tissues that hold bones in place. When they fail, those bones shift out of place, leading to a deformity. This deformity causes malalignment of the foot bones, which leading puts more stress on the already failing ligaments. This snowball effect of degeneration can significantly affect how you move.
What causes posterior tibial tendon dysfunction?
The cause of posterior tibial tendon dysfunction is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot.
Children nearly fully grown can end up with flatfeet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs.
Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur.
People who have recurring posterior tibial tendonitis (inflammation of the posterior tibial tendon) are at greater risk of developing posterior tibial tendon dysfunction.
What are the stages of posterior tibial tendon dysfunction?
Posterior tibial tendon dysfunction is divided into stages by most foot and ankle specialists:
- Stage I – Pain is present along the posterior tibial tendon without deformity or collapse of the arch. The patient has the somewhat flat or normal-appearing foot they have always had.
- Stage II – A deformity from the condition has started to occur, resulting in some collapse of the arch, which may or may not be visible or noticeable to you or others. You may experience it as simply a feeling of weakness in your arch. Many patients don't realize they have a problem until stage II, because the ligament failure can occur at the same time as the tendon failure and therefore deformity can begin at the same time that pain in the tendon is first being felt.
- Stage III – The deformity has progressed to the extent where the foot becomes fixed (rigid) in its deformed position.
- Stage IV – In this, most severe, stage, the deltoid ligament on the inside of the ankle fails, resulting in a deformity in the ankle as well as a deformity in the foot. Over time, this can lead to arthritis of the ankle.
How is posterior tibial tendon dysfunction treated?
Nonsurgical treatments
The first treatment is to support the medial longitudinal arch (the arch that spans the underside of your foot). This relieves strain on the soft tissues of the medial (inside) portion of your foot. The most effective way provide to support to relieve pain on the tendon is to use a walking boot or brace. Once the tenderness and pain goes away, an orthotic device may alleviate symptoms and may slow the progression of deformity, particularly if it is mild. However, the deformity may progress despite the use of orthotics. A boot, brace, or orthotic has not been shown to correct or even prevent the progression of the foot deformity.
Flatfoot surgery
Surgery is usually necessary if you experience persistent pain and/or have a significant deformity. Sometimes the foot just feels weak, and the assessment of deformity is best done by a foot and ankle specialist. If surgery is appropriate, a combination of soft tissue and bony procedures may be considered to correct alignment and support the medial arch, taking strain off failing ligaments.
Depending upon the tissues involved and extent of deformity, the foot and ankle specialist will determine the necessary combination of procedures, which may include one more the following types of foot surgery:
- Medial slide calcaneal osteotomy – to correct position of the heel
- Lateral column lengthening – to correct position in the midfoot
- Medial cuneiform osteotomy or first metatarsal-tarsal fusion – to correct elevation of the medial forefoot.
- Posterior tibial tendon reconstruction (tendon transfer) – grafting a healthy tendon or portion of tendon from another part of the body to replace the dysfunctional tendon.
In severe stage III cases, surgical reconstruction may include fusing bones of the hindfoot (rear portion of the foot). This results in stiffness of the hindfoot but achieves the desired pain relief.

