Tommy John Surgery

Injuries to the elbow's ulnar collateral ligament (UCL) are common among competitive overhead throwing athletes and those doing combat-type sports. Baseball players, especially, are susceptible to UCL tears. Until 1974, when the first UCL reconstruction was performed on Major League Baseball player Thomas ("Tommy John") Edward John Jr., such tears were usually career-ending injuries.
Since that time, the treatment of these injuries – including UCL reconstruction – has evolved significantly, and it can help most athletes get back to doing what they love.
What is Tommy John surgery?
Tommy John surgery (UCL reconstruction) is a complete reconstruction of the ulnar collateral ligament (UCL) in the elbow. The UCL stabilizes the inside of the elbow, and an intact ligament is essential for throwing mechanics of overhead throwing athletes. Therefore, UCL reconstruction is most commonly performed after an athlete’s dominant arm sustains a high-grade injury to the ligament.
A graft from the patient’s forearm or hamstring tendon is used to replace the damaged ligament. This provides a new, strong ligament that can allow a full return to throwing.
Who is a good candidate for Tommy John surgery?
Any healthy, overhead-throwing athlete with a complete tear or high-grade partial tear to the UCL of the elbow and who wishes to return to competition is a good candidate for Tommy John surgery. Additionally, those with lower grade injuries to the ligament who have failed conservative treatment are good candidates as well.
How does Tommy John surgery work?
Tommy John surgery begins with harvesting the tendon that will become the new ligament. This is obtained from either an extra tendon in the patient’s forearm or from one of the hamstring tendons.
Next, the torn ligament is identified. Drill holes are then created in the forearm bone (ulna) and the arm bone (humerus) at the point where the UCL normally attaches. The graft is then sutured and threaded through these holes to create a figure-8 graft.
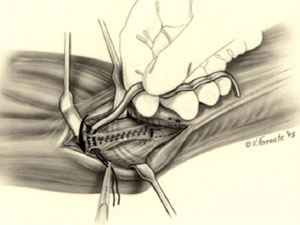
Illustration showing insertion of the tendon graft
The sutures are tied together to tighten the graft in the appropriate position. While there are dozens of variations described since the original procedure was performed on Tommy John, the three main techniques include the figure-8 technique, the docking technique (described by Dr. David Altchek) and, more recently, the anatomic technique developed by Drs. Josh Dines and Christopher Camp.
As mentioned above, when it was originally described, Tommy John Surgery or UCL reconstruction meant using a tendon graft to create a new ligament, similar to what is done during ACL reconstruction surgery of the knee. More recently, there is renewed interest in repairing the ligament, avoiding the use of grafting a tendon.
This is referred to as a UCL repair, however, some patients still refer to this as Tommy John Surgery. There are benefits to ligament repair, including the lack of needing a graft and a quicker return to play. However, it is critical to choose patients appropriately when indicating one for this procedure. Not all tear types are amenable to this.
Even more recently, the addition of non-absorbable suture to the repair or reconstruction construct has occasionally been used with good results. This addition to the procedure is referred to as an internal brace, and it is done to strengthen the construct allowing the elbow to tolerate higher loads when throwing.
How long does Tommy John surgery take?
Tommy John surgery typically takes about 45 minutes to perform. It can sometimes take longer if there are other injuries that need to be addressed at the time of surgery. Concurrent procedures (those that may be performed at the same time) can include elbow arthroscopy to remove bone spurs or decompression/transposition of the ulnar nerve. The surgeon will make this decision based upon the patient’s history and physical examination.
What are the potential risks of Tommy John surgery?
The risks of Tommy John surgery are very low, though there are some important ones to consider. The ulnar nerve is close to the surgical site. It is protected at all times, though there is a low risk of injury to the nerve. Other risks of surgery include infection, fracture of the bone, numbness around the incision, or future injury to the new ligament.
What does the recovery from Tommy John surgery look like?
After surgery, the patient will be given an elbow brace that restricts range of motion to protect the reconstruction. This is usually worn for 6 weeks while slowly increasing range of motion. Physical therapy will start soon after the procedure depending on surgeon preference with specific protocols for range-of-motion progression. Assuming they are progressing well, most baseball players will start a gradual return to throwing around the 4- to 5- month mark after surgery.
How long until you can return to sports after Tommy John surgery?
Return to competition largely depends on the sport and position played by the athlete. Most athletes begin a throwing program by 4 to 5 months after surgery. In baseball, pitchers may return to full throwing capacity 12 to 14 months after surgery, although it can sometimes take longer. Position players can return to competition sooner, typically 9 to 12 months after surgery.
What is the success rate of Tommy John surgery?
Tommy John surgery is very reliable and has a success rate of over 90% (with a return-to-play-rate of about 80% to 95%). Younger patients, especially, have low risk of complications or the need for revision surgery. The docking technique for Tommy John surgery was developed at HSS by Dr. David Altchek, and this technique has provided a strong and reliable method to help athletes return to competition.
Do you throw faster after Tommy John surgery?
Some players do throw faster after Tommy John surgery. This is often credited to physical therapy to strengthen the arm and the fact that the athlete once again has a strong ligament that can allow maximum effort throwing without pain. Another key factor here is that, in many cases, during the first 4 to 5 months after surgery when the athletes haven’t returned to throwing yet, they are able to focus on performance training for other things that often get neglected, such as lower extremity and core strengthening, shoulder range of motion, etc.
Can you strengthen your UCL?
There is some emerging research that suggests the ulnar collateral ligament can thicken from throwing and exercise. We are still learning the appropriate balance of exercise and rest to allow for optimal UCL strength. Most importantly, to prevent injury, one can work on shoulder and elbow range of motion and strengthening while at the same time being smart about the amount one throws using strict pitch counts.
Can you heal your UCL without surgery?
Some UCL injuries can heal without surgery. This largely depends on the location and the severity of the injury. Low grade injuries to the proximal UCL have the best chance of healing without surgery. High grade injuries or injuries to the distal UCL are less likely to heal on their own. A doctor with expertise in managing UCL injuries will be able to develop an appropriate treatment plan. When conservative treatment is indicated, cessation from throwing, physical therapy and even platelet-rich plasma (PRP) injections have been shown to play beneficial roles in healing.
Move Better Podcast on Tommy John surgery
Join HSS sports medicine surgeons David Altchek, James ("Beamer") Carr, and Josh Dines as they discuss UCL injuries, UCL repair and Tommy John Surgery.
Click or tap the "play" icon to listen on this page, the title to open it in Spotify, or visit the Move Better Podcast page to find this series on your preferred podcast platform.
In the news
- Dr. David Altchek, Mets doctor and Tommy John surgeon, dies at 68
- Sports Medicine Surgeon Explains Spencer Strider's Surgery and What Comes Next
- What Tommy John surgery looks like today: Revision surgeries, internal brace procedures
- After 50 years, Tommy John surgery is evolving to increase success and sometimes speed return
- Dr. James Carr from HSS Florida on the Epidemic of the UCL Tear & Tommy John's Surgery in the MLB
- Q&A: What’s next for Shohei Ohtani and the Angels in the wake of his torn UCL?
- MLB continues to be stricken with nightmare epidemic: Elbow injuries
- Jonathan Villar lands on injured list after Mets played three games shorthanded
- Players, experts, and doctors agree: Rob Manfred is putting pitchers in harm’s way with new sticky stuff regulations
- ESPN West Palm Tonight 5/27/2021
- Elbow injuries in active people
- New Study Examines Effects of Mound vs. Flat Ground Pitching in High School Pitchers
- Yankees starter Luis Severino needs Tommy John surgery
Tommy John Surgery Success Stories
Medically reviewed by James B. Carr II, MD ; Joshua S. Dines, MD ; Stephen Fealy, MD
References
- Apostolakos JM, Lin KM, Carr JB 2nd, Bedi A, Camp CL, Dines JS. The Role of Biologic Agents in the Non-operative Management of Elbow Ulnar Collateral Ligament Injuries. Curr Rev Musculoskelet Med. 2020 Aug;13(4):442-448. doi: 10.1007/s12178-020-09637-9. PMID: 32388723; PMCID: PMC7340701.
- Camp CL, Bernard C, Benavitz B, Konicek J, Altchek DW, Dines JS. Reconstruction of the Medial Ulnar Collateral Ligament of the Elbow: Biomechanical Comparison of a Novel Anatomic Technique to the Docking Technique. Orthop J Sports Med. 2019 Jul 17;7(7):2325967119857592. doi: 10.1177/2325967119857592. PMID: 31763343; PMCID: PMC6852368.
- Camp CL, Desai V, Conte S, Ahmad CS, Ciccotti M, Dines JS, Altchek DW, D'Angelo J, Griffith TB. Revision Ulnar Collateral Ligament Reconstruction in Professional Baseball: Current Trends, Surgical Techniques, and Outcomes. Orthop J Sports Med. 2019 Aug 14;7(8):2325967119864104. doi: 10.1177/2325967119864104. PMID: 31453203; PMCID: PMC6696849.
- Camp CL, Dines JS, Voleti PB, James EW, Altchek DW. Ulnar Collateral Ligament Reconstruction of the Elbow: The Docking Technique. Arthrosc Tech. 2016 May 23;5(3):e519-23. doi: 10.1016/j.eats.2016.02.013. PMID: 27656372; PMCID: PMC5021527.
- Carr JB 2nd, Camp CL, Dines JS. Elbow Ulnar Collateral Ligament Injuries: Indications, Management, and Outcomes. Arthroscopy. 2020 May;36(5):1221-1222. doi: 10.1016/j.arthro.2020.02.022. Epub 2020 Feb 27. PMID: 32112818.
- Clark NJ, Desai VS, Dines JD, Morrey ME, Camp CL. Nonreconstruction Options for Treating Medial Ulnar Collateral Ligament Injuries of the Elbow in Overhead Athletes. Curr Rev Musculoskelet Med. 2018 Mar;11(1):48-54. doi: 10.1007/s12178-018-9458-3. PMID: 29335854; PMCID: PMC5825339.
- Conti MS, Camp CL, Elattrache NS, Altchek DW, Dines JS. Treatment of the ulnar nerve for overhead throwing athletes undergoing ulnar collateral ligament reconstruction. World J Orthop. 2016 Oct 18;7(10):650-656. doi: 10.5312/wjo.v7.i10.650. PMID: 27795946; PMCID: PMC5065671.
- Degen RM, Camp CL, Bernard JA, Dines DM, Altchek DW, Dines JS. Current Trends in Ulnar Collateral Ligament Reconstruction Surgery Among Newly Trained Orthopaedic Surgeons. J Am Acad Orthop Surg. 2017 Feb;25(2):140-149. doi: 10.5435/JAAOS-D-16-00102. PMID: 28098706.
- Dines JS, Jones KJ, Kahlenberg C, Rosenbaum A, Osbahr DC, Altchek DW. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med. 2012 Jan;40(1):148-51. doi: 10.1177/0363546511422350. Epub 2011 Sep 16. PMID: 21926384.
- Erickson BJ, Carr J, Chalmers PN, Vellios E, Altchek DW. Ulnar Collateral Ligament Tear Location May Affect Return-to-Sports Rate but Not Performance Upon Return to Sports After Ulnar Collateral Ligament Reconstruction Surgery in Professional Baseball Players. Am J Sports Med. 2020 Sep;48(11):2608-2612. doi: 10.1177/0363546520947090. Epub 2020 Aug 18. PMID: 32809845.
- Jensen AR, LaPrade MD, Turner TW, Dines JS, Camp CL. The History and Evolution of Elbow Medial Ulnar Collateral Ligament Reconstruction: from Tommy John to 2020. Curr Rev Musculoskelet Med. 2020 Jun;13(3):349-360. doi: 10.1007/s12178-020-09618-y. PMID: 32314245; PMCID: PMC7251039.
- Johnson CC, Garcia GH, Liu JN, Stepan JG, Patel RM, Dines JS. Internet resources for Tommy John injuries: what are patients reading? J Shoulder Elbow Surg. 2016 Dec;25(12):e386-e393. doi: 10.1016/j.jse.2016.07.073. Epub 2016 Oct 10. PMID: 27745805.
- Jones KJ, Dines JS, Rebolledo BJ, Weeks KD, Williams RJ, Dines DM, Altchek DW. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014 Jan;42(1):117-21. doi: 10.1177/0363546513507695. Epub 2013 Oct 21. PMID: 24145949.
- Kunze KN, Fury MS, Pareek A, Camp CL, Altchek DW, Dines JS. Biomechanical Characteristics of Ulnar Collateral Ligament Injuries Treated With and Without Augmentation: A Network Meta-analysis of Controlled Laboratory Studies. Am J Sports Med. 2024 Feb 2:3635465231188691. doi: 10.1177/03635465231188691. Epub ahead of print. PMID: 38304942.
- Meyers KN, Middleton KK, Fu MC,, Dines JS. Comparison of a Novel Anatomic Technique and the Docking Technique for Medial Ulnar Collateral Ligament Reconstruction. Am J Sports Med. 2022 Mar;50(4):1061-1065. doi: 10.1177/03635465221076149. Epub 2022 Feb 21. PMID: 35188812.
- Moran J, Kammien A, Cheng R, Amaral JZ, Santos E, Modrak M, Kunze KN, Vaswani R, Jimenez AE, Gulotta LV, Dines JS, Altchek DW. Low Rates of Postoperative Complications and Revision Surgery After Primary Medial Elbow Ulnar Collateral Ligament Repair. Arthrosc Sports Med Rehabil. 2024 Jan 19;6(1):100828. doi: 10.1016/j.asmr.2023.100828. PMID: 38313860; PMCID: PMC10835117.
- Osbahr DC, Dines JS, Rosenbaum AJ, Nguyen JT, Altchek DW. Does posteromedial chondromalacia reduce rate of return to play after ulnar collateral ligament reconstruction? Clin Orthop Relat Res. 2012 Jun;470(6):1558-64. doi: 10.1007/s11999-011-2132-3. PMID: 22009711; PMCID: PMC3348298.
- Rebolledo BJ, Dugas JR, Bedi A, Ciccotti MG, Altchek DW, Dines JS. Avoiding Tommy John Surgery: What Are the Alternatives? Am J Sports Med. 2017 Nov;45(13):3143-3148. doi: 10.1177/0363546517692548. Epub 2017 Mar 9. PMID: 28278401.
- Redler LH, Degen RM, McDonald LS, Altchek DW, Dines JS. Elbow ulnar collateral ligament injuries in athletes: Can we improve our outcomes? World J Orthop. 2016 Apr 18;7(4):229-43. doi: 10.5312/wjo.v7.i4.229. PMID: 27114930; PMCID: PMC4832224.
- Vaswani R, White A, Dines J. Medial Ulnar Collateral Ligament Injuries in Contact Athletes. Curr Rev Musculoskelet Med. 2022 Dec;15(6):474-482. doi: 10.1007/s12178-022-09785-0. Epub 2022 Aug 2. PMID: 35917095; PMCID: PMC9789220.
