Scoliosis
Summary: Scoliosis is a complex orthopedic condition in which the spine curves sideways. It can begin in childhood, adolescence or adulthood. This article by HSS physicians explains the types, causes, signs and symptoms of scoliosis, and how it is diagnosed. Finally, it covers nonsurgical treatment options such as bracing and physical therapy – including the Schroth Method – to advanced surgical correction through multi-level spinal fusion.

On this page:
What is scoliosis?
Scoliosis is a condition of the spine in which the spine curves sideways in an "S" shape, either to the right or left side. This is different from the condition known as kyphosis, where the spine has an abnormal, forward-oriented curvature. However, scoliosis and kyphosis often occur together.
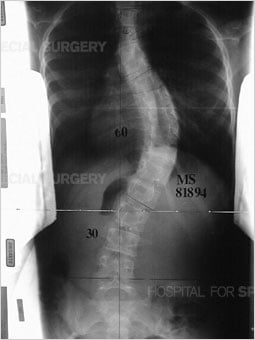
Anteroposterior (front-to-back) view of the spine in standing position, demonstrating scoliosis (sideways curvature).

Lateral (outer side) view of the spine in standing position, demonstrating kyphosis (forward curvature).
What are the signs and symptoms of scoliosis?
The key symptom in all forms of scoliosis is a sideways curvature of the spine. This is usually revealed when a shoulder, waist, hip other body part is higher on one side than on the other. Back pain is common in people who develop scoliosis as an adult, but rare among children and adolescents. When a child or teenager with scoliosis does experience back pain, this may be a sign that they have some additional condition.
A diagnosis for scoliosis made if a sideways curvature in the spine exceeds 10 degrees. In adults, this curve usually exceeds 30 degrees before they seek treatment.
Scoliosis animation
This video provides an animated illustration of juvenile and adult scoliosis.
What causes scoliosis?
Scoliosis is usually idiopathic (cause unknown). However, in some patients it is congenital (present at birth), caused by degeneration of the spinal joints or discs, or caused by a neuromuscular condition unrelated to structures of the bone.
Basic types of scoliosis
- Idiopathic scoliosis: The cause or origin is unknown. This is the most common type of scoliosis. It is diagnosed most often in teenagers (known as adolescent idiopathic scoliosis). When scoliosis develops for unknown reasons in adults who have no history of the condition, this is called de novo scoliosis.
- Congenital scoliosis: Bones in the spine are abnormally curved sideways at birth.
- Neuromuscular scoliosis: The curvature is a symptom of a separate, systemic condition affecting the nervous system and/or muscular system, such as cerebral palsy, neurofibromatosis, muscular dystrophy, paralysis. This type of scoliosis often creates complex curvatures, such as an overlapping kyphosis condition. (Learn more about neuromuscular scoliosis.)
- Degenerative scoliosis: Affecting older adults, this type of scoliosis is caused by wear and tear on spinal joints or discs. (Learn more by reading Degenerative Scoliosis: Causes, Symptoms, Diagnosis, Treatment.)
- Syndromic: For example, scoliosis is found in people who have Marfan syndrome or Ehlers-Danlos syndrome.
These conditions are all types of what is termed "structural scoliosis," where incorrectly formed bones create an S-curve in the spine that is fixed and cannot be straightened by adjusting body position.
"Nonstructural scoliosis" (also known as "functional scoliosis") is where the curvature is temporary and not caused by a malformed vertebrae in the spine but by a separate condition that affects posture, such as skeletal dysplasia or a leg length discrepancy.
Scoliosis can affect the spine in any of its three major sections:
- cervical spine (neck)
- thoracic spine (chest and upper back region)
- lumbar spine (lower back)
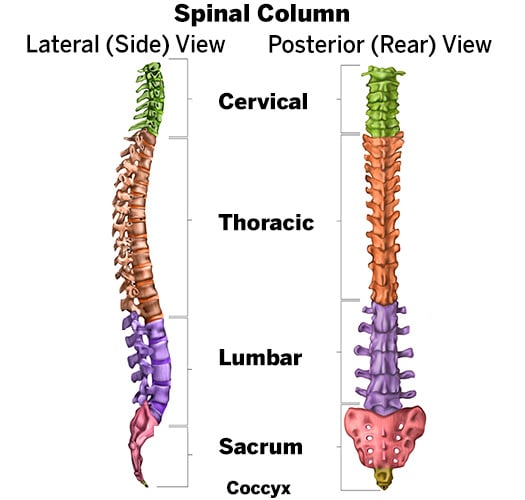
Diagram showing the sections of the healthy spine, with the neck (cervical) section at the top, followed below by the thoracic and lumbar sections, the sacrum and the coccyx (tailbone). The curvature shown in the left image is the normal curve of the spine when it is viewed from the side (not scoliosis).
Who gets scoliosis?
Scoliosis is primarily diagnosed in children and adolescents. Adolescent idiopathic scoliosis is the type of scoliosis seen most frequently by spine surgeons, representing 80% of all spinal deformity cases.
- Scoliosis affects girls much more than boys, by a ratio of about 8 to 1.
- Almost one in three people who get scoliosis a family history of this condition.
- About 2% of teenagers get scoliosis.
Far less often, scoliosis can affect adults. This may be due either to a progression of a curve that existed in their youth but went was not either diagnosed or treated at the time, or it be the result of a degenerative spine condition or osteoporosis. Learn more about adult scoliosis by reading Scoliosis In Adults: Symptoms, Diagnosis and Treatments.
How is scoliosis diagnosed?
Typically, scoliosis is first noticed by a child’s pediatrician, family member or school nurse. As an initial screening method, healthcare professionals use the Adams forward-bending test to look for the presence of any asymmetry of the torso or shoulder blades, or for protrusion of the shoulder blades. The medical evaluation for scoliosis includes a physical exam and spinal imaging.
During the Adams forward bending test, a doctor may use a scoliometer to measure the amount of trunk inclination. A child or adolescent with an inclination measuring 7 degrees or greater will often be referred to an orthopedist for further evaluation with an X-ray and monitoring.

This photo shows a pronounced curve, revealed during an Adams forward-bending test.
To assess the curve further, X-ray images or low-dose radiation EOS images are taken from the front and side views. Parents who are concerned about exposing their child to radiation during medical imaging should consult a doctor to learn whether EOS imaging is an appropriate alternative to traditional X-rays. EOS imaging has several safety and diagnostic advantages, especially for children or teens who may need to have multiple images taken over time to monitor the progression of their scoliosis.
What kind of doctor treats scoliosis?
The appropriate specialist depends on the patient's age. Children and adolescents should consult a pediatric orthopedic surgeon with expertise in spine conditions. Adults should consult an orthopedic spine surgeon or physiatrist (a nonsurgical doctor specializing in physical medicine). Complete care for any patient will usually be provided by an integrated healthcare team, including a doctor or surgeon, one or more physical therapists and, if bracing is needed, an orthotist.
Consulting with a surgeon does not necessarily mean you will need to have surgery. In mild cases affecting kids and teenagers, especially, the pediatric orthopedist may first wish only to monitor the spinal curve over time to determine whether treatment will be needed. In other cases, bracing and/or rehabilitation early on may eliminate the need for surgery. Only an orthopedic spine surgeon or pediatric orthopedic surgeon should perform surgery for scoliosis.
Led by the highly specialized orthopedic surgeons at the Lerner Children's Pavilion and HSS Spine, HSS is recognized as a world leader in the management of complex spinal deformities in both children and adults. Find an HSS doctor who treats scoliosis.
What is the treatment for scoliosis?
Treatments may be surgical or nonsurgical, and they also vary depending on the type of scoliosis a person has, and the age at which they develop it.
The treatment for adolescent idiopathic scoliosis is determined by the degree of the spinal curve at the time of diagnosis and by the anticipated progression of that curve. Mild cases may not require any treatment. More significant cases may be treated nonsurgically, using braces, or with spinal fusion surgery.
Nonsurgical treatment of adolescent idiopathic scoliosis
For curves measuring less than 25 degrees, the orthopedist may recommend frequent monitoring to determine whether additional intervention becomes necessary.
Young people with curves between 25 and 45 degrees may be candidates for treatment with bracing. While bracing does not correct the curve, it has been shown to stop progression in up to 75% of patients. Bracing is considered a success when progression is halted and maintained within 6 degrees of the original measurement of the curve.
In most cases, patients wear a brace for 18 hours a day, removing it only for hygiene and sports activities. However, some patients may only require the use of a brace at night.
A variety of braces are available, and the selection of which is based on how many curves are present and where on the spine the curve or curves are located. Some models provide support at the pelvis, front, back and neck, while others provide support throughout the torso and underarms.
While many braces are rigid, flexible braces have been developed in recent years. This type of brace, which is only appropriate in patients with single curves, is worn as a vest and allows the patient to participate in some sports activities.
Patients continue to wear the brace until they have stopped growing and skeletal maturity is reached. This allows the supportive muscles in the patient's back and trunk to become stronger after a period of inactivity. Physical therapy is sometimes recommended.
The Schroth Method
The Schroth Method is a physical therapy and exercise treatment that can be used in scoliosis patients of all ages. The goal is to elongate the trunk and correct imbalances of the spine by developing the inner muscles of the rib cage. In this treatment, a physical therapist with specialized training teaches the patient specific exercises and corrective breathing techniques to straighten de-rotate the spine. (Learn more in The Schroth Method: A Specialized Treatment for Scoliosis.)
Surgical treatment of adolescent idiopathic scoliosis
Patients with curves that continue to progress beyond 50 degrees, either with or without bracing, generally require surgical intervention.
How does scoliosis surgery work?
There are different surgical methods, but the most common type of surgery is a posterior spinal fusion with instrumentation (artificial implants). In this procedure, the orthopedic surgeon makes an incision from the back and essentially "welds" the vertebrae together using bone chips.
These bone chips may be:
- autografts – taken from elsewhere in the patient's own body
- allografts – sourced from donors through a bone bank
The spine is then healed in alignment by hooks or screws and rods. Once the fusion is complete, the implants no longer serve a function but are left in place to avoid the need for additional surgery. Some patients may be candidates to have a surgical fusion using minimally invasive spine surgery.
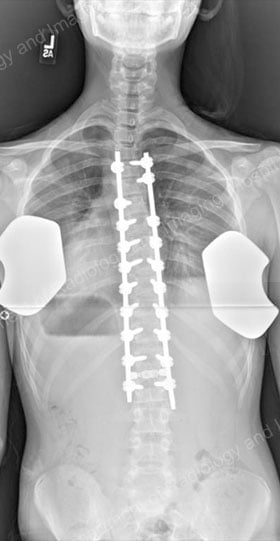

Postsurgical X-ray images of the corrected spine, with a posterior (rear) view and a lateral (outer side) view.
What is the recovery time for scoliosis surgery?
Most spinal fusion patients stay in the hospital for three to five days and are working with a physical therapist and standing within a day of surgery. Children and teens can usually return to school in four to six weeks and return to full activity at three months. The complete healing process may take 6 to 12 months.
Patients who undergo combined anterior and posterior spine procedures may have a slightly longer stay in the hospital. Nevertheless, recovery times from modern scoliosis spine surgeries are significantly shorter than they were decades ago, when people sometimes spent weeks or months in the hospital in a body cast or in traction.
What are the risks of scoliosis surgery?
Rare complications of spinal fusion for scoliosis can include infection and spinal cord abnormalities or injury. The procedure provides significant spine curvature correction, cosmetic and posture benefits, but does cause some inflexibility in the spine.
Risk prevention
At HSS, multiple precautions are taken during surgery to mitigate risks and protect the patient. These include the administration of antibiotics during surgery to help guard against infection and continuous monitoring of sensory and motor function of the spinal cord.
Curvature correction
Fusion surgery generally yields very good results, with a correction rate of between 60% to 100%, depending on curve flexibility and location. Spinal fusion does result in some loss in range of motion, however. The extent of that loss varies depends on the section of spine corrected and the number of vertebrae that are fused.
Cosmetic results
- a balanced spine
- leveled shoulders
- reduction or elimination of any rib hump
Will scoliosis get better without treatment?
Scoliosis cannot correct itself on its own, but not all patients will need treatment. Only about 5% of children or adolescents with scoliosis require bracing or surgery. In some cases, the progression of the curvature can just be monitored over time. If your pediatrician or family doctor suspects your child has scoliosis, however, it is important to get an assessment by an appropriate specialist as soon as possible. Early intervention, such as bracing, may prevent the need for a patient to have surgery later in life.
Get more detailed information about scoliosis by exploring the articles and other content below, or find an HSS physician who treats scoliosis.
Key takeaways
- Scoliosis is a sideways curvature of the spine that can affect people of all ages, but is most commonly diagnosed in adolescents.
- There are several types of scoliosis, including idiopathic (unknown cause), congenital (present at birth), neuromuscular (linked to other conditions), degenerative (age-related), and syndromic (associated with genetic disorders).
- Early detection is important, especially in children and teens. Screening often begins with a visual and physical exam, including a forward-bending test, followed by imaging such as X-rays or low-dose-radiation EOS scans.
- Symptoms vary and may include uneven shoulders, back pain, or visible curvature – although some people with mild cases may be symptom-free.
- Treatment depends on the severity of the curve and the patient’s age. Options include observation, bracing, physical therapy (such as the Schroth Method), or surgery.
- Bracing can stop scoliosis from progressing in many adolescents, especially when it is begun while they are still growing. Most braces are worn 18 hours per day.
- Surgery, typically spinal fusion, is considered when curves exceed 50 degrees or continue to progress despite bracing. Modern surgical techniques are more effective and have shorter recovery times than those of the past.
Scoliosis Success Stories
Medically reviewed by John S. Blanco, MD ; Shevaun Mackie Doyle, MD ; Jessica H. Heyer, MD ; Roger F. Widmann, MD
References
- Dolan LA, Weinstein SL, Dobbs MB, Flynn JMJ, Green DW, Halsey MF, Hresko MT, Krengel WF 3rd, Mehlman CT, Milbrandt TA, Newton PO, Price N, Sanders JO, Schmitz ML, Schwend RM, Shah SA, Song K, Talwalkar V. BrAIST-Calc: Prediction of Individualized Benefit From Bracing for Adolescent Idiopathic Scoliosis. Spine (Phila Pa 1976). 2024 Feb 1;49(3):147-156. doi: 10.1097/BRS.0000000000004879. Epub 2023 Nov 23. PMID: 37994691; PMCID: PMC10841822.
- Smith JS, Kelly MP, Yanik EL, Baldus CR, Buell TJ, Lurie JD, Edwards C, Glassman SD, Lenke LG, Boachie-Adjei O, Buchowski JM, Carreon LY, Crawford CH, Errico TJ, Lewis SJ, Koski T, Parent S, Lafage V, Kim HJ, Ames CP, Bess S, Schwab FJ, Shaffrey CI, Bridwell KH. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis at 5-year follow-up: durability of outcomes and impact of treatment-related serious adverse events [published online ahead of print, 2021 Apr 30]. J Neurosurg Spine. 2021;1-13. doi:10.3171/2020.9.SPINE201472
- Yang JH, Kim HJ, Chang DG, Suh SW. Comparative Analysis of Radiologic and Clinical Outcomes Between Conventional Open and Minimally Invasive Scoliosis Surgery for Adolescent Idiopathic Scoliosis [published online ahead of print, 2021 Apr 15]. World Neurosurg. 2021;S1878-8750(21)00565-9. doi:10.1016/j.wneu.2021.04.025
- Alhammoud A, Alborno Y, Baco AM, Othman YA, Ogura Y, Steinhaus M, Sheha ED, Qureshi SA. Minimally Invasive Scoliosis Surgery Is a Feasible Option for Management of Idiopathic Scoliosis and Has Equivalent Outcomes to Open Surgery: A Meta-Analysis [published online ahead of print, 2021 Feb 9]. Global Spine J. 2021;2192568220988267. doi:10.1177/2192568220988267
