Patellofemoral Center
Patellofemoral injuries and conditions like “runner’s knee” and dislocations can affect anyone and cause debilitating pain or instability of the kneecap (patella) without proper treatment.
The physicians at the Patellofemoral Center at HSS specialize in the management of kneecap pain and deterioration, as well as the surgical interventions that can help you heal and regain mobility. Using the latest technology and increasingly less invasive methods, our specialists offer their many years of experience diagnosing and treating patients to provide optimal care for your specific needs.
Advanced Treatments and Research for Patellofemoral Conditions
Meet the Team
Our physicians are devoted to performing, researching, and teaching the latest techniques and treatments for patellofemoral conditions.
Surgeons
Physicians
Physical Therapists
Patellofemoral Disorders
The knee is a complex structure. Explore the various indications for kneecap surgery, minimally invasive alternatives, and more.
Learn about the various conditions and treatments that affect the patellofemoral joint.
Video Series
Dr. Strickland
- Patella (Kneecap) Instability
- Patellar Pain and Arthritis
- Knee Chondromalacia, Arthritis, and Tendonitis
- Anterior Cruciate Ligament (ACL)
- Tibial Tubercle
- Tibial Tubercle Osteotomy Patient Testimonial
- MPFL Reconstruction
- Regenerative Medicine – PRP and Stem Cells
- MACI – Repair Knee Cartilage Defects Using Your Own Cells
Animations
MPFL Reconstruction Animation
Patellofemoral Joint Replacement Video
Facebook Live Discussion
Condition Articles
- Patellofemoral Disorders: An Overview
- Patellofemoral Arthritis: Diagnosis and Treatment
- Patellofemoral Pain Syndrome
- Patellofemoral Instability
- Medial Patellofemoral Ligament (MPFL) Reconstruction
- Tibial Tubercle Transfer
- Kneecap Cartilage Surgery
- Patellofemoral Joint (PFJ) Replacement
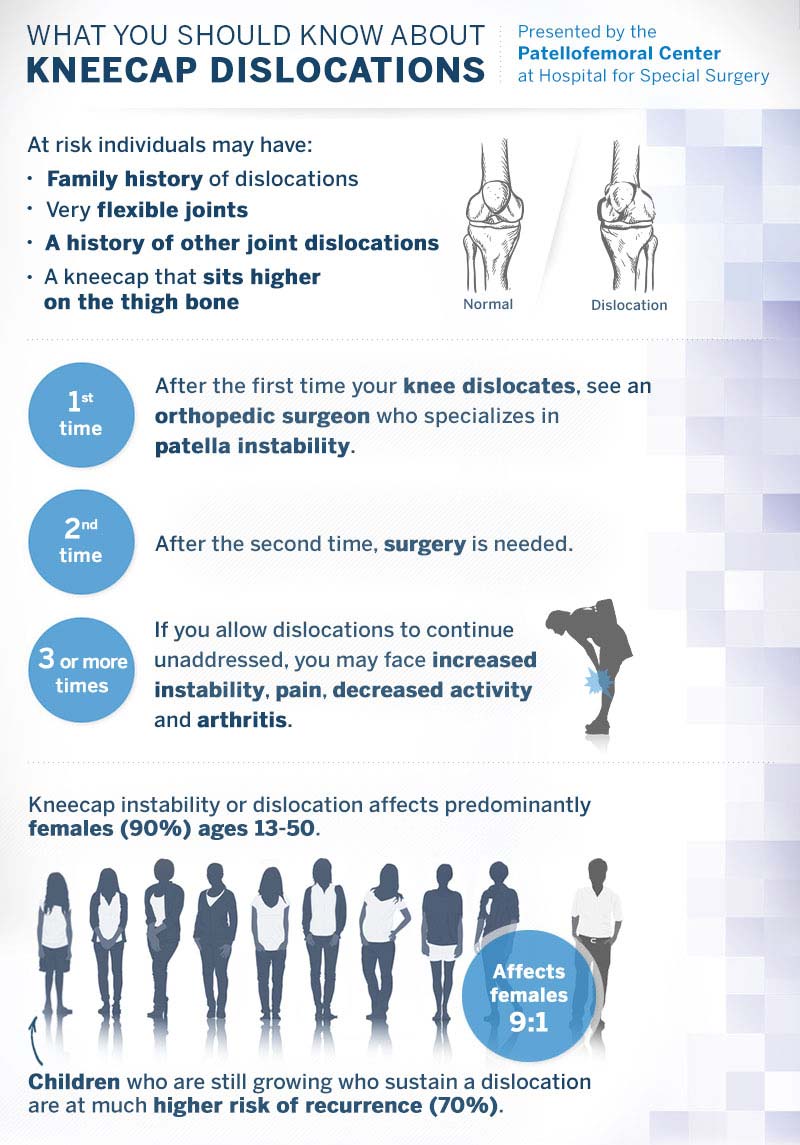
Kneecap Dislocation Infographic
Patellofemoral Center Research Program
More than four million Americans are affected by pain due to kneecap injuries. See how facts and research have informed our treatments, care, and rehabilitation methods.
Patellofemoral disorders, also known as kneecap disorders, refer to pain and instability issues arising from a variety of sources in the patellofemoral joint. Some common examples include anterior knee pain, osteoarthritis and recurrent dislocations or subluxations. These disorders are multifactorial in etiology and can greatly inhibit patients from maintaining their active lifestyles. Furthermore, these conditions affect patients of a wide range of ages and activity, although this population is predominantly female. Patients, physicians and physical therapists find the diagnosis and treatment of these conditions extremely challenging. Currently, patients with anterior knee pain, instability and arthritis have great difficulty understanding their problem and finding the correct clinician to treat their pathology. Many orthopaedic caregivers see these conditions frequently in their offices, though treatment is extremely variable.
Our group addresses the current lack of formalized research into patellofemoral disorders, treatments and outcomes. Our Patellofemoral Center focuses on clinical outcome studies in order to evaluate current surgical techniques as well as develop new ones and improve patient outcomes. The Center has taken a comprehensive approach to investigating patient outcomes in a variety of patellofemoral disorders and treatment procedures. By utilizing a combination of prospective, retrospective, and biomechanical projects our group assesses the efficacy of current procedures and improves upon them to develop even better treatment options. The Patellofemoral Center is also focused on conducting collaborative research efforts with other institutions in the form of multi-center studies in order to maximize the quality and power of the patellofemoral patient data available. The comprehensive research efforts of the Patellofemoral Center play a critical role in improving the quality of life of the many patients suffering from knee pain and instability.
The specific areas of investigation include:
- Analysis of factors that may help predict failure of patella stabilizing surgery
- Comparison of surgical versus non-surgical treatment in first time dislocators with open growth plates
- Evaluation of isolated medial patellofemoral ligament reconstruction to treat instability in the knee
- Evaluation of the effect of current surgical techniques on contact mechanics and pressures of different trochlear and patellar morphologies
- Evaluation of juvenile particulated cartilage to improve severe cartilage defects in the patella.
- Determining the effect of patellofemoral surgery on patella vascularity
- Measuring outcomes and quality of life in patients undergoing PFJ arthroplasty
- Determining outcomes including return to sport after MPFL reconstruction
- Evaluating tibial tubercle transfers in the management of patellar pain and arthritis
Support for our center helps us carry out our research program. Specific areas that can be supported include:
- Clinical research personnel including research assistants, coordinators, and biostatisticians
- Engineering support including biomechanical analysis, robotic testing, TekScan sensors, 3D printing, and cadaveric specimens
- Imaging such as MRI, ultrasound and x-rays and histology
- Advanced technologies including registry platforms and software programs that streamline data entry, storage, and analysis
- Research staff and technologies required to facilitate large multi-institution studies
Papers, Awards and Bibliography
- Green DW, Arendt EA, Wixted C, Price M. Quadriceplasty Techniques for Patellar Stabilization. In: Patellar Instability: Management Principles and Operative Techniques, 1st ed. USA: Wolters Kluwer; 2019: 123-133. [ISBN: 978-1496380821].
- Green DW, Price MJ, Quadricepsplasty Operative Techniques. In: Patellar Instability: Management Principles and Operative Techniques, 1st ed. USA: Wolters Kluwer; 2019: [ISBN: 978-1496380821].
- Green DW, Wixted C, Price M, Parikh SN. Pediatric Distal Stabilization Procedures. In Patellar Instability: Management Principles and Operative Techniques, 1st ed. USA: Wolters Kluwer; 2019: 323-336. [ISBN: 978-1496380821].
- Green DW, Price MJ, Moloney J. Patellofemoral Pain in the Skeletally Immature Patient: Diagnosis and Treatment. In: Patellofemoral Pain and Instability: Etiology, Diagnosis and Management. Switzerland: Springer; 2019: 3-25. [978-3319976396].
- Uppstrom, TJ, Price M, Black S, Gausden E, Haskel J, Green DW. Medial Patellofemoral Ligament (MPFL) Reconstruction Technique Using an Epiphyseal Femoral Socket with Fluoroscopic Guidance Helps Avoid Physeal Injury in Skeletally Immature Patients. Knee Sur Sports Traumatology Arthroscopy. 2019 Mar. 9. doi: 10.1007/s00167-019-05412-7. [Epub ahead of print]. PMID: 30852626
- Gruskay J, Strickland S, Casey E, Chiaia T, Green D, Gomoll A. Team Approach: Patellofemoral Instability in the Skeletally Immature. JBJS Reviews. 2019: 1-32. doi: 10.2106/JBJS.RVW.18.00159.
- Richmond CG, Green DW, Cannamela PC, Martinson D, Shea KG. The Distance Between the Hamstring Grafts and the Physis and Apophysis of the Proximal Tibia – Implications for Pediatric ACL Reconstruction and Physeal Arrest. J of ISAKOS. 2018 Sep 3. DOI: 10.1136/jisakos-2018-000222.
- Price MJ, Tuca M, Nguyen J, Silberman J, Luderowski E, Uppstrom TJ, Green DW. Juvenile Osteochondritis Dissecans of the Trochlea: A Cohort Study of 34 Trochlear Lesions Associated With Sporting Activities that Load the Patellofemoral Joint. J Ped Ortho. 2018 Apr. 16. DOI: 10.1097/BPO.0000000000001174. [Epub ahead of print]; PMID: 29664877.
- Keyes S, Price M, Green DW, Parikh SN. Special Considerations for Pediatric Patellar Instability. Am J of Ortho. 2018 Mar. 27; 2018;47(3). DOI: 10.12788/ajo.2018.0017; PMID: 29611848.
- Strickland S, Bird Mackenzie, Christ A. “Advances in Patellofemoral Arthroplasty,” Curr Rev Musculoskelet Med. June 2018; 11(2): 221-230.
- Wang D, Shubin Stein B, Strickland S. (2018). Patellofemoral Issues. Farr J & Gomoll A (Eds.), Cartilage Restoration: Practical Clinical Applications 2nd Edition. 103-117. Springer Science.
- Christ AB, Koch C, Shubin Stein BE, Gonzalez Della Valle A, Strickland SM. “Patellofemoral arthroplasty conversion to total knee arthroplasty: Retrieval analysis and clinical correlation” The Knee. October 2017; 24(5): 1233-1239.
- Liu JN, Steinhaus ME, Kalbian IL, Post WR, Green DW, Strickland SM, Shubin Stein BE. Patellar Instability Management: A Survey of the International Patellofemoral Study Group. Am J Sports Med. 2017 Oct. 1:363546517732045. DOI: 10.1177/0363546517732045. [Epub ahead of print]; PMID: 28985094.
- Liu J, Steinhaus M, Kalbian I, Post W, Green D, Strickland S, Shubin Stein, B. “Patellar Instability Management: A Survey of the International Patellofemoral Study Group.” American Journal of Sports Medicine. October 2017; 46(13): 3299-3306.
- Grawe B, Burge A, Nguyen J, Strickland S, Warren R, Rodeo S, Shubin Stein B. “Cartilage Regeneration in Full-Thickness Patellar Chondral Defects Treated with Particulated Juvenile Articular Allograft Cartilage: An MRI Analysis” Cartilage. October 2017; 8(4): 374-383.
- Brady JM, Sullivan JP, Nguyen J, Mintz D, Green DW, Strickland S, Shubin Stein BE. The Tibial Tubercle-to-Trochlear Groove (TT-TG) Distance is Reliable in the Setting of Trochlear Dysplasia and Superior to the Tibial Tubercle-to-Posterior Cruciate (TT-PCL) Distance When Evaluating Coronal Malalignment in Patellofemoral Instability. Arthroscopy. 2017 Aug. 25. DOI: 10.1016/j.arthro.2017.06.020. [Epub ahead of print]; PMID: 28847574.
- Nwachukwu B, So C, Schairer W, Shubin Stein B, Strickland S, Green D, Dodwell E. “Economic Decision Model for First-Time Traumatic Patellar Dislocations in Adolescents.” American Journal of Sports Medicine. August 2017; 45(10): 2267-2275.
Liu J, Strickland S, Shubin Stein B. “Patellar Instability Management: A Survey of the International Patellofemoral Study Group.” American Journal of Sports Medicine. July 2017. - Liu J, Mintz D, Nguyen J, Munch J, Strickland S, Shubin Stein B. “MRI Validation of Tibial Tubercle Transfer Distance: A Clinical and Cadaveric Study” July 2017.
- Benedict Nwachukwa, Conan So, William Schairer, Beth Shubin-Stein, Sabrina Strickland, Daniel Green, Emily Dodwell. Economic Decision Model for First-Time Traumatic Patellar Dislocations in Adolescents. Am J Sports Med. 2017.
- Grawe B, Rodeo S, Burge A, Strickland S, Warren R, Nguyen J, Shubin Stein B. “Patellar Chondral Defects Treated with Particulated Juvenile Articular Allograft Cartilage: An MRI Analysis.” Podium presentation at: 2016 International Cartilage Repair Societ. 2016 September 24-27; Naples, Italy.
- Munch J, Sullivan J, Nguyen J, Mintz D, Green D, Shubin Stein B, Strickland S. “Patellar Articular Overlap is a Simple Alternative to Conventional Measurements of Patellar Height.” Orthopaedic Journal of Sports Medicine. July 2016.
- Uppstrom TJ, Haskel JD, Gausden EB, Meyer R, Shin YW, Nguyen JT, Green DW. Reliability of Predictive Models for Non-Operative Healing Potential of Stable Juvenile Osteochondritis Dissecans Knee Lesions. Knee. 2016 Aug. DOI: 10.1016/j.knee.2016.03.005.
- Redler L, Mayer G, Kalbian I, Nguyen J, Shubin Stein B, Strickland S. “Does Ligamentous Laxity Protect Against Chondral Injury in Patients with Patellofemoral Instability?” Poster presentation at: 2016 American Orthopaedic Society for Sports Medicine Annual Meeting. 2016 July 7-10; Colorado Springs, CO.
- Christ A, Baral E, Koch C, Shubin Stein B, Della Valle A, Strickland S. “Patellofemoral arthroplasty conversion to total knee arthroplasty: retrieval analysis and clinical correlation.” Poster presentation at: 2016 European Society of Sports Traumatology, Knee Surgery, and Arthroscopy Annual Meeting. 2016 May 4-7; Barcelona, Spain.
- Munch J, Sullivan J, Nguyen J, Mintz D, Green D, Strickland S, Shubin Stein B. “MRI Measurements Associated with Patellofemoral Instability.” Podium Presentation at: 2016 European Society of Sports Traumatology, Knee Surgery, and Arthroscopy Annual Meeting. 2016 May 4-7; Barcelona, Spain.
- Johnson A, Shubin Stein B, Mintz D, Demehri S, Wolfe L, Cosgarea A. “Complications Following Tibial Tuberosity Osteotomy With and Without Distalization.” Poster presentation at: 2016 Arthroscopic Association of North America Annual Meeting. 2016 April 14-16; Boston, MA.
- Liu J, Mintz D, Nguyen J, Munch J, Strickland S, Shubin Stein B. “MRI Validation of Tibial Tubercle Transfer Distance: A Clinical and Cadaveric Study.” Poster presentation at: 2016 Arthroscopic Association of North America Annual Meeting. 2016 April 14-16; Boston, MA.
- Nwachukwu BU, So C, Schairer WW, Green DW, Dodwell ER. Surgical versus Conservative Management of Acute Patellar Dislocation in Children and Adolescents: A Systematic Review. Knee Surg Sports Traumatology Arthroscopy. 2016 Mar.; 24(3):760-7. DOI: 10.1007/s00167-015-3948-2. Review.
- Redler L, Meyers K, Munch J, Dennis E, Nguyen J, Shubin Stein B. “Anisometry of Medial Patellofemoral Ligament Reconstruction in the Setting of Patella Alta and Increased Tibial Tubercle-Trochlear Groove (TT-TG) Distance.” Podium presentation at: 2016 American Orthopaedic Society for Sports Medicine Annual Meeting. 2016 July 7-10; Colorado Springs, CO.
- Redler L, Strickland S, Shubin Stein B. “Patellofemoral Arthroplasty”. Master Techniques in Orthopaedic Surgery: Reconstructive Knee Surgery 4th Edition. In press.
- Green DW. Surgical Treatment of Pediatric Patella Instability. In: Die Therapie Der Instabilen Patella. Zurich: AGA-Komitee-Knie-Patellofemoral; 2016: 80-90.
- Shin YW, Trehan SK, Uppstrom TJ, Widmann RF, Green DW. Radiographic Results and Complications of Three Guided Growth Implants. J Ped Ortho. 2016
- Munch JL, Sullivan JP, Nguyen JT, Mintz D, Green DW, Shubin Stein BE, Strickland S. Patellar Articular Overlap on MRI is a Simple Alternative to Conventional Measurements of Patellar Height. Ortho. J Sports Med. 2016 4(7).
- Uppstrom TJ, Gausden EB, Green DW. Classification and Assessment of Juvenile Osteochondritis Dissecans Knee Lesions. Curr Opin Ped. 2016; 28(1):60-7.
- Green DW. Editor. Pediatric and Adolescent Knee Surgery. USA: Wolters Kluwer Health; 2015
- Green DW, Gausden EB. Medial Patellofemoral Ligament Reconstruction: Hamstring Technique. In: Pediatric and Adolescent Knee Surgery. USA: Wolters Kluwer Health; 2015: 140-147. [ISBN: 978-1451193350].
- Green DW, Uppstrom TJ, Haskel JD. Bioabsorbable Fixation of Symptomatic Juvenile Osteochondritis Dissecans Lesions in Children and Adolescents. In: Pediatric and Adolescent Knee Surgery. USA: Wolters Kluwer Health; 2015: 207-212. [ISBN: 978-1451193350].
- Green DW, Haskel JD, Shin YW. Applications of Implant-Mediated Guided Growth in Pediatric Knee Surgery. In: Pediatric and Adolescent Knee Surgery. USA: Wolters Kluwer Health; 2015: 327-335. [ISBN: 978-1451193350].
- Gausden EB, Fabricant PD, McCarthy MM, Taylor SA, Weeks KD, Potter H, Green DW. MPFL Reconstruction in Children and Adolescents: A review of Surgical Indications and Treatment Options. JBJS Reviews. 2015; 3(10).
- Green DW, Ladenhauf HN. Perspective: MPFL Reconstruction with Hamstring Autograft. Orthopaedics Today – Europe. Jun. 2014. Pages 72-73
- Lurie B, Koff MF, Parina S, Feldman E, Amacker N, Zayas TD, Widmann RF, Green DW, Potter HG. Three-Dimensional Magnetic Resonance Imaging of Physeal Injury: Reliability and Clinical Utility. Journal of Ped Ortho. 2014; Apr.-May; 34(3):239-45.
- Fabricant PD, Ladenhauf HN, Salvati EA, Green DW. Medial Patellofemoral Ligament (MPFL) Reconstruction Improves Radiographic Measures of Patella Alta in Children. Knee. 2014 Dec.; 21(6)1180-4. DOI: 10.1016/j.knee.2014.07.023. Epub 2014 Jul. 30.
- Fabricant PD, Robles A, Downey-Zayas T, Do HT, Marx RG, Widmann RF, Green DW. Development and Validation of a Pediatric Sports Activity Rating Scale: The Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS Pedi-FABS). Am J Sports Med. 2013 Oct.; 41(10):2421-9. Epub 2013 Jul. 26.
- Patellofemoral Research Excellence Award. 2016. Arthroscopy Association of America/Patellofemoral Foundation. Awarded to an outstanding research project leading to improved understanding, prevention and treatment of patellofemoral pain or instability for “Anisometry of Medial Patellofemoral Ligament Reconstruction in the Setting of Patella Alta and Increased Tibial Tubercle-Trochlear Groove (TT-TG) Distance.”
- Fellow Research Award — Clinical Science. 2016. American Orthopaedic Society for Sports Medicine. Awarded to the best papers in clinical science and basic science submitted by a sports medicine fellow for “Anisometry of Medial Patellofemoral Ligament Reconstruction in the Setting of Patella Alta and Increased Tibial Tubercle-Trochlear Groove (TT-TG) Distance.”
- Patellofemoral Research Excellence Award. 2015. Arthroscopy Association of America/Patellofemoral Foundation. Awarded to an outstanding research project leading to improved understanding, prevention and treatment of patellofemoral pain or instability for “MRI Measurements Associated with Patellofemoral Instability.”
- Philip D. Wilson, MD Award. 2015. Hospital for Special Surgery. Awarded to a fellow for excellence in orthopaedic surgery research for “Anisometry of Medial Patellofemoral Ligament Reconstruction in the Setting of Patella Alta and Increased Tibial Tubercle-Trochlear Groove (TT-TG) Distance.”
- Excellence in Research Award. American Orthopaedic Society for Sports Medicine Development and Validation of a Pediatric Sports Activity Rating Scale. AOSSM Annual Meeting 2013.
- AOSSM Herodicus Award Nominee Podium Presentation MRI Evaluation of the Medial Patella-Femoral Ligament (MPFL) After Acute Patellar Dislocation in Children. 2010.
- Jacques Duparc Award presented at the EFORT Meeting (European Federation of National Orthopaedics and Traumatology) for the study Zone of Injury of the Medial Patella-femoral Ligament After Acute Patellar Dislocation in Children and Adolescents. 2010.
- Outcomes After Isolated Medial Patellofemoral Ligament Reconstruction for the Treatment of Recurrent Lateral Patellar Dislocations: A Systematic Review and Meta-analysis (pdf). Daniel K. Schneider, Brian Grawe, Robert A. Magnussen, Adrick Ceasar, Shital N. Parikh, Eric J. Wall, Angelo J. Colosimo, Christopher C. Kaeding and Gregory D. Myer. Am J Sports Med published online February 12, 2016.
- Widespread Implementation of Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Instability Maintains Functional Outcomes at Midterm to Long-Term Follow-up While Decreasing Complication Rates: A Systematic Review (pdf). Kristen L. Stupay, BA, Eric Swart, MD, and Beth E. Shubin Stein, MD. Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 31, No 7 (July), 2015: pp 1372-1380
- Epidemiology of Patellofemoral Instability Injuries Among High School Athletes in the United States (pdf). Joshua Mitchell, Robert A. Magnussen, Christy L. Collins, Dustin W. Currie, Thomas M. Best, R. Dawn Comstock and David C. Flanigan. Am J Sports Med (2015) 43: 1676.
- Patellofemoral arthroplasty: outcomes and factors associated with early progression of tibiofemoral arthritis (pdf). D.L. Dahm, M.M. Kalisvaart, M.J. Stuart, S.W. Slettedahl. Knee Surg Sports Traumatol Arthrosc (2014) 22:2554–2559.
- Predictors of Recurrent Instability After Acute Patellofemoral Dislocation in Pediatric and Adolescent Patients (pdf). Laura W. Lewallen, Amy L. McIntosh and Diane L. Dahm. Am J Sports Med (2013) 41: 575
- The Clinical Outcome of Patellofemoral Arthroplasty (pdf). Jess H. Lonner, MD, Michael R. Bloomfield, MD. Orthop Clin N Am 44 (2013) 271–280.
- Patellofemoral Instability in Athletes: Treatment via Modified Fulkerson Osteotomy and Lateral Release (pdf). Fotios Paul Tjoumakaris, Brian Forsythe and James P. Bradley. Am J Sports Med (2010) 38: 992.
- Correlation of Patellar Articular Lesions with Results from Anteromedial Tibial Tubercle Transfer (pdf). Arthur J. Pidoriano, MD, Richard N. Weinstein, MD, David A. Buuck, MD, and John P. Fulkerson, MD. Am J Sports Med (1997) 25: 4.
Meet our team and learn about their expertise
Why choose HSS? Our patients say it best.
Back to Sports Medicine Institute