Managing Spine Complications in a 28-year-old Woman with Spondyloepiphyseal Dysplasia Congenita Indicated for Total Hip Arthroplasty
From Grand Rounds from HSS: Management of Complex Cases | Volume 14, Issue 2
Case Report
A 28-year-old woman with spondyloepiphyseal dysplasia congenita (SEDc) was referred to the Kathryn O. and Alan C. Greenberg Center for Skeletal Dysplasias (CSD) at HSS with worsening right hip pain that would “catch” with activities, as well as left hip and right shoulder pain. Her height was 4′ 3.5″, and her surgical history included posterior cervical spine fusion (C1–C2) at 6 years old to treat instability.
At the CSD, she underwent genetic counseling and molecular genetic testing to confirm the SEDc diagnosis and rule out a lysosomal storage disease such as Morquio syndrome, which can present as skeletal phenocopies with different extraskeletal risks that affect anesthesia management and cardiopulmonary safety. A dominant variant in the COL2A1 gene was detected, confirming the clinical SEDc diagnosis [1].
This case report details her treatment at HSS for conditions related to SEDc: os odontoideum in the cervical spine in Part 1 and severe, degenerative arthrosis of the right hip in Part 2.
Part 1: Revision Posterior Cervical Spine Fusion
Spine X-rays showed thoracolumbar scoliosis and a hypoplastic dens with instability at C1–C2, the prior surgical site, with no posterior bony fusion mass (Figure 1). Computed tomography (CT) scanning showed os odontoideum and nonunion of the prior surgery (posterior cerclage wire extended to a small fragment of bone, just anterior to the posterior arch of C1, which was not otherwise united to the remainder of the posterior arch of C1). Non-contrast magnetic resonance imaging (MRI) showed severe central canal stenosis at C1–C2 with impingement of the posterior aspect of the spinal cord and myelomalacia, as well as thoracic scoliosis with flattened vertebral bodies and no significant lumbar spinal stenosis (Figure 2).
Figure 1. Preoperative X-ray shows instability at C1–C2, as well as the prior surgical site.
Figure 2: Non-contrast MRI shows severe central canal stenosis at C1–C2.
Due to the significant C1–C2 instability and to facilitate intraoperative monitoring during surgery, the patient agreed to undergo revision posterior cervical spine fusion before undergoing total hip arthroplasty (THA). She is right hand dominant and experienced no fine motor changes in her upper extremities, nor did she experience issues with balance or other signs of myelopathic changes or spine compression. Her physical examination showed 5/5 strength in all muscle groups and intact sensation. Biceps and quadriceps reflexes were 3+. Hoffman sign was negative, and the toes were downgoing.
Following administration of general anesthesia, Gardner-Wells tongs were placed and the patient was placed in a prone position on the Jackson table. After sterile prepping and draping, an incision was made from posterior occiput to C3, incorporating the scar from prior surgery. Subperiosteal dissection of the spinous process and of the lamina of C2 and the posterior section of C1 was carried out laterally on the ring of C1, approximately 12 to 15 mm from the midline on either side. After identifying the pars at C2, the surgeon identified the undersurface of the C1 lateral mass. The greater occipital nerve was sacrificed bilaterally to gain adequate exposure to the area, and the posterior cervical wire from the prior fusion was removed. C1 lateral mass screws were placed using a drill at the mid aspect of the C1 lateral mass, aimed slightly superiorly. The drill tract was palpated and found to have a solid anterior wall, and the C1–C2 joints were decorticated with a high-speed bur and C2 laminar screws were placed. Using a bur, a starting hole was made in the spinous process, and unicortical drilling was performed through the spinous process to the lamina bilaterally. Again, the holes were palpated and a solid anterior cortex was found.
The surgeon placed C1 screws (3.5 mm in diameter and 28 mm in length) and C2 screws (3.5 mm in diameter, 22 mm in length on the left, and 3.5 mm in diameter and 30 mm in length on the right). Fixation was excellent. A sponge soaked with bone morphogenetic protein-2 (BMP-2) was packed into the decorticated facet joints bilaterally. Contoured rods and cross connectors were used to secure the instrumentation, end caps were placed, and the wound was closed.
Immediately after surgery she was neurologically intact and was discharged home on postoperative day 1. She wore a cervical collar for 3 months. At 11 months postoperatively, cervical spine X-ray with flexion and extension views showed no evidence of instability (Figure 3). The patient was approved for THA.
Figure 3: Postoperative X-ray shows no signs of cervical instability.
Part 2: Bilateral Total Hip Arthroplasty
While the patient healed from the cervical spine fusion, she reported stiffness, catching and locking of both hips, a feeling of instability, and pain that interfered with sleep and worsened with activity. Steroid injections and physical therapy had not alleviated her symptoms. Crutches eased the pain of weightbearing and she walked with a coxalgic gait.
On physical examination she could passively flex the hip joints to 90°, with severe pain on straight-leg raise with resistance and no internal or external rotation of the right hip and minimal on the left. Anteroposterior supine pelvic and whole body X-rays showed generalized osteopenia and severe, degenerative arthrosis, with bone-on-bone apposition of the right hip and remodeling of the left hip with near bone-on-bone apposition (Figure 4). She was indicated to undergo bilateral, staged THA—the right hip first and the left 4 months later.
Figure 4: AP pelvic and whole body X-rays showed osteopenia and severe arthrosis of the hips.
With the patient positioned laterally, a computer navigation system was used to place 2 pins in the iliac crest for the pelvic camera, used to record initial pelvic position. A longitudinal incision was made over the posterior corner of the greater trochanter, exposing the lateral aspect of the femur and the short external rotators. A posterior capsulotomy was performed after release of the pirifomis and the conjoined tendon from the posterior femur and elevation of the gluteus minimus. The hip was dislocated, and the neck was cut as templated.
Acetabular retractors were placed and the labrum was excised. After the acetabulum was reamed, the 48-mm acetabular cup was placed at 40° inclination and 20° anteversion, guided by bony landmarks and computer navigation, and fixed with 2 screws (Figure 5). The dual mobility liner was seated, and osteophytes were removed from the acetabular rim.
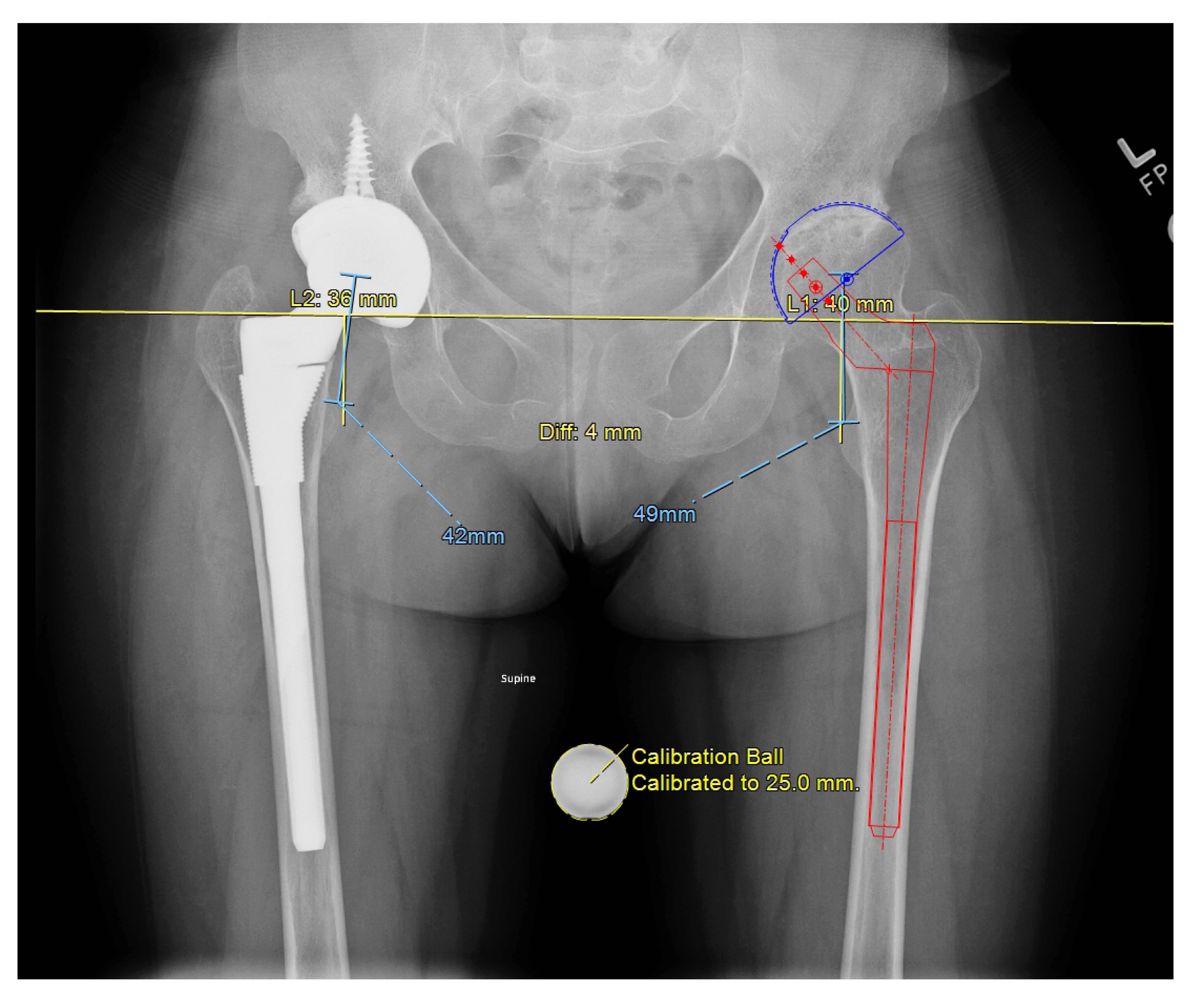
Figure 5: Guided by bony landmarks and computer navigation, a 48-mm acetabular cup was placed at 40° inclination and 20° anteversion.
Femoral retractors were placed proximally for exposure, and soft tissue was removed from the pirifomis fossa. The femoral canal was opened using a box osteotome followed by reaming of the femoral canal to the templated size. The hip was taken through range of motion and was stable. Next, the hip was dislocated, the trial implant was removed, and the final femoral implants and dual mobility head constructs were impacted into place. On the left side, 2 cerclage wires were placed below and above the lesser trochanter due to osteopenia. After the acetabulum was irrigated and suctioned, the hips were reduced with good overall stability and satisfactory leg length.
The patient was discharged home on postoperative day 2 for each arthroplasty, weightbearing as tolerated on the right and 20% toe-touch weightbearing with crutches due to osteopenia on the left. At 3 months postoperatively from the second of the staged procedures, the patient reported minimal discomfort. She walked independently and could reciprocate stairs (Figure 6).
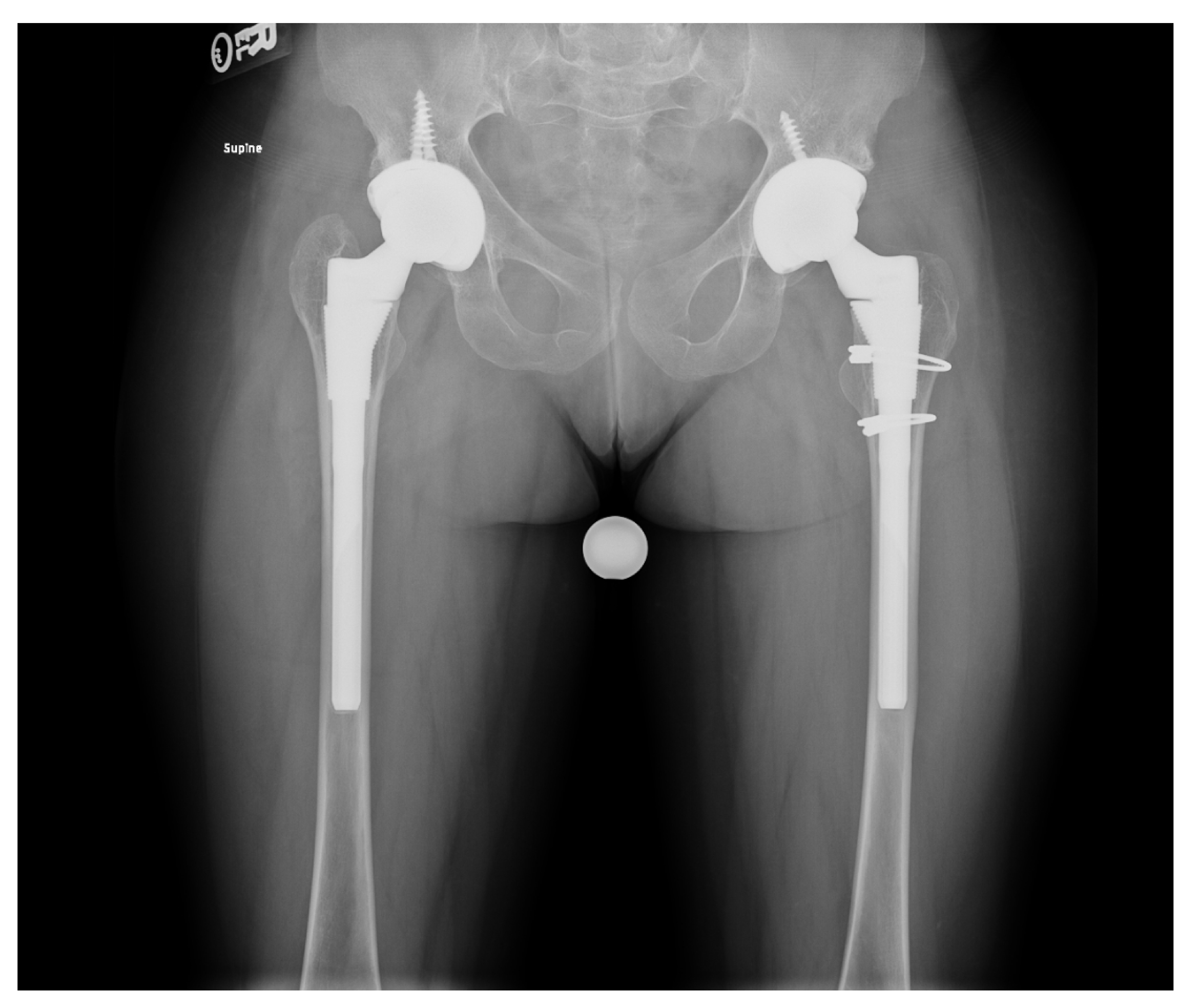
Figure 6: Postoperative AP views.
Discussion
This case illustrates the complex nature of diagnosing and treating patients with musculoskeletal manifestations of SEDc, a genetic disorder characterized by early-onset osteoarthritis and spine anomalies [2], a disproportionately short trunk and barrel-shaped chest; a short neck, knock-knees, average-size hands and feet, and short stature (average adult height, 2′ 11″ to 4′ 9″). Some individuals have orofacial conditions such as midface hypoplasia or cleft palate, and there is a risk of both hearing loss and myopia, which is rarely associated with retinal detachment. Individuals tend to be flexible, and the muscles may have low tone. Motor development may be delayed, but mental development is normal.
Adults may develop bowed legs and early-onset osteoarthritis, which may require joint replacement [3], as well as odontoid abnormalities, scoliosis, and abnormally shaped vertebrae. Spine complications and risk for atlantoaxial instability in SEDc require careful preoperative evaluation in all patients undergoing surgery; risks for nonskeletal morbidities should be evaluated in balancing the risks and benefits of surgery [4].
References
- Barat-Houari M, Sarrabay G, Gatinois V, et al. Mutation update for col2a1 gene variants associated with type ii collagenopathies. Hum Mutat. 2016;37(1):7-15. doi: 10.1002/humu.22915.
- Unger S, Ferreira CR, Mortier GR, et al. Nosology of genetic skeletal disorders: 2023 revision. Am J Med Genet A. 2023;191(5):1164-1209. doi:10.1002/ajmg.a.63132.
- Carter EM, Raggio CL. Genetic and orthopedic aspects of collagen disorders. Curr Opin Pediatr. 2009;21(1):46-54. doi: 10.1097/mop.0b013e32832185c5.
- Savarirayan R, Bompadre V, Bober MB, et al.; Skeletal Dysplasia Management Consortium. Best practice guidelines regarding diagnosis and management of patients with type II collagen disorders. Genet Med. 2019;21(9):2070-2080. doi: 10.1038/s41436-019-0446-9.



