This center offers virtual care. To schedule a virtual visit, please call this center directly.
Osteoporosis and Metabolic Bone Health Center
Metabolic bone disease refers to abnormalities in bones caused by a broad spectrum of disorders. Conditions that are often considered metabolic bone disorders include osteoporosis, osteomalacia, rickets, hypophosphatemia, and Paget’s disease. Most commonly, these disorders are caused by abnormalities of minerals such as calcium, phosphorus or vitamin D. Some of these disorders have a genetic basis. The HSS Osteoporosis and Metabolic Bone Health Center cares for patients with these types of disorders and consists of physicians and nurse practitioners in the fields of orthopedics, endocrinology, rheumatology and women’s health.
ISCD Accreditation
In addition to the standard bone density test, our center can perform trabecular bone score, body composition, vertebral fracture assessment and atypical femoral fracture assessment bone scan. HSS is the only facility in the state of New York that is certified by the International Society for Clinical Densitometry (ISCD). All scans are performed by dedicated, certified full-time DXA technologists. Patients can meet with a nurse practitioner to review test results and discuss a treatment plan that may include calcium, vitamin D and exercise program and perhaps medication.
Our physicians



10 Steps to Better Bone Health
It is never too late to lower your fracture risk. Several factors contribute to an individual's risk of a fracture, and these need to be addressed together in order to have the maximum benefit. Many patients are confused about how these different factors will impact their bone. This brochure intends to provide basic information and general guidelines. Please talk to your doctor about questions and to obtain specific information.
Osteoporosis is a bone disease, which is characterized by weak bones that are at risk for breaking (fracturing). Even though osteoporosis does not cause symptoms, it is important to treat. Patients who have osteoporosis are at risk for breaking a bone even with a small amount of force in placed on the bone, such as tripping on the sidewalk. Healthy bones should not break if you fall from standing height. That indicates that there is a problem with the strength of your bones.
By treating osteoporosis, we can lower an individual's risk of having a fracture. The consequences of a fracture can be devastating. Fractures can be extremely painful. They can interfere with a person’s quality of life, independence, ability to care for oneself and live alone. In the first year following a hip fracture, 25% of people will die from complications. Many more people are unable to walk or get about unassisted after a major fracture.
Certain risk factors for osteoporosis are not modifiable and cannot be changed. These include genetic factors (for example if a parent had a hip fracture). Several medical conditions and medications have negative effects on bone. Having these conditions when you are young can have a lasting impact on your skeleton, which is often not reversible. Treating the underlying illness is often beneficial to bone. When possible, the lowest doses and shortest courses of medications which have harmful effects on bone should be utilized. These options should be discussed with your doctor.
1. Understand your fracture risk
- Osteoporosis can be diagnosed based on a history of a low trauma or a bone density test.
- Bone density is measured by DXA which is short for dual-energy x-ray absorptiometry.
- DXA scales bone mineral density in relation to what would be expected for a young, healthy adult. Based upon how much lower your bone density is in relation to the young reference patient you will receive a classification as “normal”, “osteopenic” (low bone mass), or “osteoporotic” (well below normal).
- Fracture risk is related not only to bone density but also to many factors that we think of as bone quality.
- Certain diseases and medications (such as steroids) have a greater impact on bone quality and so can raise fracture risk even if bone density is normal. In some cases additional tests of bone quality can be helpful.

2. Obtain Adequate Calcium
- Calcium is one of the most important components of healthy bones.
- The Institute of Medicine recommends 1200 mg of calcium per day for postmenopausal women (age > 50 years old) and men older than 70, and 1000 mg of calcium per day for women 19-50 years old and men 19-70.
- Total calcium intake should be from diet and supplements combined.
- It is best to obtain as much calcium as possible from diet and only use supplements as needed in addition to reach recommended goals.
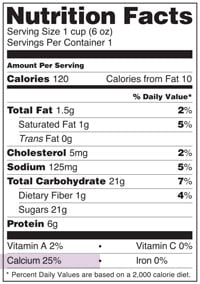
- The foods richest in calcium are generally dairy products.
- Look at food labels to see how much calcium is in a given product.
- To determine the mg if calcium in a given food, multiply the percent of RDA on the label by 100 (i.e. 25% of RDA is equivalent to 250 mg).
- Calcium Supplementation.
- There are two common types of calcium supplements: citrate and carbonate:
- Calcium carbonate must be taken with food for proper absorption and should not be used in patients taking medications that block stomach acid (proton pump inhibitors).
- Calcium citrate can be taken with or without food.
- A serving of calcium citrate is often two or more pills, so always check labels carefully.
- The body can only absorb 500-600 mg of calcium at a time so calcium doses should be spaced throughout day by at least 4 hours.
- There are two common types of calcium supplements: citrate and carbonate:
- More is not better – excess doses of calcium can cause medical problems including kidney stones and constipation. While there is some evidence tying high doses of calcium supplements to cardiac disease this is not conclusive. However, moderate doses and obtaining as much calcium as possible from diet is the best option.
3. Obtain Adequate Vitamin D
- The Institute of Medicine recommends 600 IU of Vitamin D per day for adults up to age 70 years and 800 IU per day for adults over age 70.
- Individual requirements vary and depend on many factors including how well vitamin D is absorbed, diet, sun exposure and body size.
- Unlike calcium, it is difficult to obtain adequate vitamin D from diet alone.
- Vitamin D does not need to be taken in divided doses. It can be taken once daily or less frequently on a weekly or twice weekly basis.
- The best indicator of vitamin D sufficiency is a blood test.
- The ideal level of vitamin D is approximately 30 ng/ml.
- Vitamin D levels should not exceed 50 ng/ml.
- While some studies have shown that vitamin D has many benefits beyond the skeleton there is no data to suggest that taking high doses of vitamin D will confer any benefit. High intakes are not recommended.
- Too much vitamin D can be harmful, high doses are associated with a greater risk of falls and fractures. In population studies levels above 50 are associated with increased morbidity and mortality.
4. Exercise
- Two types of exercise are important for building bone and maintaining bone health, weight bearing and resistance exercise.
- Weight bearing exercise means exercise that involves working against gravity while your body is upright.
- Includes walking, stair climbing, dancing, jogging and running.
- Resistance exercise includes using light weights, exercise bands, weight machines. These help improve muscle strength and prevent falls.
- If you have osteoporosis at the spine, talk to your doctor or a physical therapist about which exercises are safe and best for you.
- Exercise has a very small effect bone density, but still has a beneficial overall effect on skeletal health.
5. Lower your fall risk
- Most fractures result from falls.
- Balance exercise and core strengthening exercises will help lower fall risk.
- Use railings when going down stairs.
- Wear low heeled shoes with rubber soles.
- Make your home safe
- Avoid small rugs and mats in your home.
- Make sure the path from bed to bathroom is free of objects that could be tripped over in the middle of the night.
- Consider grab bars in the shower/bath.
6. Maintain a healthy weight
- In premenopausal women having a very low body weight can interfere with estrogen production which negatively impacts bone .
- In postmenopausal women, low body weight is also a risk factor for fracture.
- Obesity is associated with abnormal bone quality and can also increase fracture risk.
- Maintaining a body weight in the normal range is optimal for bone health .
7. Avoid tobacco
- Smoking cigarettes speeds bone loss.
- Current use of tobacco use is an independent risk factor for fracture.
8. Limit alcohol
- Excessive amounts of alcohol directly harm bone cells.
- More than 2 alcoholic beverages per day is associated with an increased risk of fracture.
9. Use osteoporosis medication if indicated
- For patients who are at low fracture risk, medication is typically not prescribed because the risk of a side effect outweighs the risk for fracture.
- For patients at high risk for fracture, treatment is recommended because the consequences of an osteoporotic fracture can be devastating.
- Fracture risk is determined by many factors including prior history of low trauma fracture, bone density, family history, other medical conditions and medication use.
- Patients may be at high risk of fracture and warrant treatment even with normal bone density if they have had a prior osteoporotic fracture or are using medications or have conditions that impact bone quality .
- It is important to realize that for patients who are at high risk for fracture, calcium, vitamin D, and exercise can be helpful in addition to medication but are not sufficient on their own.
- Currently available treatments have different mechanisms of action. They work by targeting different parts of the cycle by which bone is built up and broken down.
- Osteoporosis medications increase bone mineral density and most importantly, significantly lower risk of fracture. They improve the quality of bone in addition to the amount of bone.
- While these medications (like all medications) have some side effects, the incidence of serious side effects is extremely rare and is most cases they are very well tolerated.
- If indicated, your doctor will explain the risks and benefits associated with each medication and help determine which medication is best for you.
10. See a metabolic bone specialist
- A metabolic bone specialist is typically an Endocrinologist or a Rheumatologist who has expertise taking care of patients with osteoporosis and other mineral and skeletal diseases.
- They can offer additional input regarding diagnosis and treatment when needed.
Research
Linda Russell
- Osteoporosis and orthopedic surgery: effect of bone health on total joint arthroplasty outcome.
- Osteoporosis and osteomalacia.
Juliet Aizer
- Fracture liaison services: promoting enhanced bone health care.
- Predictors of bone density testing in patients with rheumatoid arthritis.
Richard S. Bockman
- Commentary on calcium supplements and cardiovascular events.
- The effects of gallium nitrate on bone resorption.
John Carrino
- Lumbar spine: reliability of MR imaging findings.
- MRI of bone marrow edema-like signal in the pathogenesis of subchondral cysts.
Dorothy Fink
Marci Goolsby
- Bone Health in Athletes.
- A displaced femoral neck stress fracture in an amenorrheic adolescent female runner.
Joseph Lane
- Metabolic bone disease and Paget's disease in the elderly. Part I: Metabolic bone disease.
- Osteoporosis: current modes of prevention and treatment.
Kevin Math
Doug Mintz
- The use osteochondral allograft in the treatment of a severe femoral head fracture.
- Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation.
Robert Schneider
- Imaging of Osteoporosis.
- Gli1+ Mesenchymal Stromal Cells Are a Key Driver of Bone Marrow Fibrosis and an Important Cellular Therapeutic Target.
Alana Serota
- Osteoporosis: differences and similarities in male and female patients.
- Bisphosphonate Drug Holiday? Celebrate?: Commentary on article by Jordan C. Villa, MD, Arianna Gianakos, BS, Jospeh M. Lane, MD Bisphosphonate Treatment in Osteoporosis: Optimal Duration of Therapy and the Incorporation of a Drug Holiday.
Emily Stein
Contact Us
To schedule an appointment with the nurse practitioner, Rhea Rey, NP, please call 212.774.7580.
To schedule a bone density appointment, call 212.224.7935.
To schedule an appointment with one of the physicians, call the physician's office directly.
In the News
- 7 Ways to Keep Your Bones Strong as You Age
- Paging the Bone Whisperers: HSS’s Metabolic Fellowship Gets $495K
- Hospital for Special Surgery Receives Distinguished Award
- Myths and Truths About Osteo and Bone Fractures
- Osteoporosis remains underdiagnosed, undertreated after periprosthetic femur fracture
- Can Breastfeeding Lead to Bone Injuries Postpartum in Runners?
- Are Breastfeeding Runners at Greater Risk of Bone Injuries?
- Diabetes Raises Your Risk of These Spine Conditions
- Do Collagen Supplements Really Make Your Skin and Bones Healthier?
- The One Exercise You Should Try Before You’re 30
- 5 Reasons Walking Is Good for Your Health
- Updated Guideline Introduces Recommendations for Prevention & Treatment of Glucocorticoid-Induced Osteoporosis
- Fall Prevention Tips By Dr. Alana Serota, Osteoporosis Expert
- Drinking Just One Cup of This Beverage Daily Helps Ensure Your Bones and Brain Stay Strong as You Age
- A beginner’s guide to Paget’s disease
- Early Trial Offers Hope Treating Rare 'Brittle Bone' Disease
- Here’s a Doctor’s Take On Why Weight Training is Necessary As We Age
- How Safe Is a 'Holiday' From Bone-Strengthening Meds?
- Lumbar Epidural Steroid Jab Lowers Bone Formation in Older Women
- All About Your Bones with Dr. Marci Goolsby & Dr. Alana Serota (Episode 53)
- MRI-based Texture Analysis of Trabecular Bone for Opportunistic Screening of Skeletal Fragility
- Short sleep after menopause linked to weaker bones
- May is National Osteoporosis Month