Parsonage-Turner Syndrome (Neuralgic Amyotrophy)
Parsonage-Turner syndrome (PTS) is a rare neuromuscular condition, predominantly involving the upper extremity. Hospital for Special Surgery is one of the few centers in the United States that has a highly specialized interdisciplinary team of radiologists, physiatrists, neurologists and peripheral nerve surgeons dedicated to diagnosis, treatment and research of this condition.

Research Studies
To learn about HSS research studies on Parsonage-Turner syndrome, please email RadNerve@hss.edu.
What is Parsonage-Turner syndrome?
Parsonage-Turner syndrome (PTS), also known as neuralgic amyotrophy or brachial neuritis, is a rare peripheral neuropathy that predominately affects one or more nerves that control movements of the chest wall, shoulder, arm, forearm and hand. PTS can affect one or both sides of the body.
PTS most commonly affects branches arising from the brachial plexus, a complex network of nerves that arise from the cervical spinal cord to control motor function and sensation throughout the upper extremity. PTS can also affect nerves in the forearm. The most commonly affected nerves are the:
- Long thoracic nerve, which supplies the serratus anterior muscle to control the scapula.
- Suprascapular nerve, which supplies the supraspinatus and infraspinatus muscle to control shoulder abduction and external rotation.
- Axillary nerve, which supplies the deltoid and teres minor muscles to control shoulder abduction and external rotation.
- Anterior interosseous nerve, which supplies the flexor pollicis longus, pronator quadratus, and flexor digitorum profundus muscles to control the thumb.
- Phrenic nerve, which supplies the diaphragm. While the phrenic nerve is less commonly affected, its involvement can cause patients to experience shortness of breath.

Muscle atrophy and scapular winging, in which the scapula (shoulder blade) sticks out, rather than remaining flat. This can result from muscle denervation of the serratus anterior, secondary to hourglass constrictions of the long thoracic nerve.
MR neurogram showing a denervation of serratus anterior muscle.
MR neurogram showing hourglass-like constrictions of the long thoracic nerve.
What are the symptoms of Parsonage-Turner syndrome?
Patients typically experience a sudden episode of extreme pain in the shoulder region, frequently during the night or early morning, that then spontaneously resolves after a few days or weeks. This is followed by significant weakness in one or more muscles of the upper extremity. However, PTS can cause signs and symptoms that may overlap with other conditions, such as cervical radiculopathy or calcific tendinosis.
Some people with PTS may also experience Kiloh Nevin syndrome, or the inability to make the "OK" sign by pressing the thumb to the forefinger. This results from neuropathy of the anterior interosseous nerve, which supplies the flexor pollicis longus, pronator quadratus, and partially, the flexor digitorum profundus.

What causes Parsonage-Turner syndrome?
The cause of PTS is largely unknown, although it may be related to inflammation mediated by the immune system and/or changes in blood circulation.
Possible genetic predisposition and triggers
Most people who get PTS have no family history of the condition, but a rare, hereditary form of PTS is recognized. A mutation in the SEPTIN-9 (SEPT9) gene has been identified as one of the contributing causes of hereditary PTS. The SEPT9 gene is active in cells throughout the body, including neurons and immune cells. Mutations in SEPT9 have also been identified in people with other hereditary neuropathies, including:
- Autoimmune or vascular triggers.
- Mechanical events (physical activity). Some patients report developing symptoms within hours of an extraordinary amount of upper extremity exertion (such as shoveling heavy snow, competing in a push-up contest, moving heavy furniture, etc.)
- Other triggers: Some patients with PTS report some “trigger” or preceding event prior to developing symptoms, such as viruses or other infections, surgery, strenuous exercise, childbirth, vaccinations, antibiotic treatments or immunotherapy.
Who gets Parsonage-Turner syndrome?
Parsonage-Turner syndrome is considered a rare disease, with estimated prevalence of 1 to 3 in 100,000 individuals. However, recent studies have estimated that its incidence may be as high as 1 in 1000.
There are some differences in the spectrum of disease between hereditary and non-hereditary forms of PTS. The average age of onset of PTS is 25 years for people with the hereditary form of PTS and 40 for people with non-hereditary PTS. There is a higher incidence of PTS in men than in women.
What type of doctor treats Parsonage-Turner syndrome?
To help people with PTS, a multidisciplinary team of specialists is often required. This may include neurologists or physiatrists who specialize in neuromuscular medicine, radiologists who specialize in peripheral nerve imaging (MR neurography, ultrasound), peripheral nerve surgeons, and physical or occupational therapists. HSS has a team of specialists who regularly see patients with Parsonage-Turner syndrome and who work collaboratively to ensure that these patients are supported in all aspects of their condition.
How is Parsonage-Turner syndrome diagnosed?
The diagnosis of PTS requires, at a minimum, a review of symptoms and a physical exam by a doctor. If PTS is then suspected, electrodiagnostic testing (including electromyography, also known as EMG testing) and advanced radiological imaging such as MR neurography can help doctors confirm the diagnosis and determine which nerves are affected.
Clinical indicators for PTS
PTS commonly presents as severe, acute pain in the shoulder region that lasts for a few days to weeks and is followed by muscle weakness.
Electrodiagnostics
Physiatrists and neurologists use electrodiagnostic testing to both confirm the diagnosis of PTS and to monitor recovery by determining the extent of nerve injury.
Diagnostic imaging
MRI can be used to rule out other potential causes of PTS-like symptoms, such as cervical radiculopathy. A high-resolution MRI technique, known as magnetic resonance nerography (MR neurography), and ultrasound imaging can also be used to determine which nerves are impacted by PTS and which muscles show denervation (loss of nerve supply). Nerves in the upper extremity affected by PTS are marked by constriction and/or twisting. These are called “hourglass-like constrictions” (also known as "intrinsic constrictions") because the squeezed nerves look like an hourglass on a digital radiological image.
The examples below demonstrate suprascapular neuropathy with weakness in the shoulder's ability for abduction and external rotation.
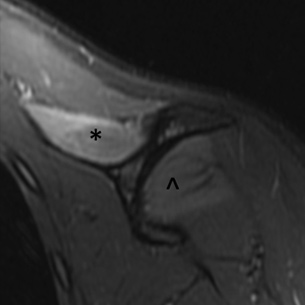
MR neurography in Parsonage-syndrome showing denervation of supraspinatus (*) and infraspinatus (^) muscles.

The location of the supraspinatus and infraspinatus muscles.
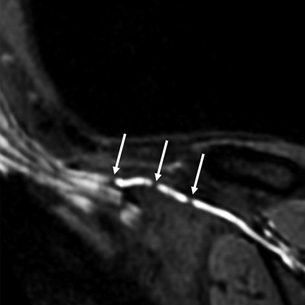
MR neurogram showing hourglass-like constrictions of superscapular nerve.
Is there a cure for Parsonage-Turner syndrome?
There is no known cure, but some treatments are available for this rare condition. These include use of oral steroids (particularly in the early stages of the condition) and physical therapy. Surgery may be considered for patients with PTS who do not recover after these measures.
Is there surgery for Parsonage-Turner syndrome?
Surgery can be helpful for patients with chronic PTS who do not show improvement with nonsurgical intervention. Microsurgical neurolysis, sometimes referred to as microneurolysis, is used to release the hourglass-like constrictions that form in affected nerves. MRI and/or ultrasound is used to precisely localize these constrictions and thereby provide a surgical roadmap. Physicians at HSS have found that, in people with chronic Parsonage-Turner syndrome, microneurolysis was associated with significantly improved clinical outcomes compared patients who had nonsurgical treatment.
Can Parsonage-Turner syndrome be treated without surgery?
Many patients eventually recover and regain function of their arm without surgery or other interventions. A damaged nerve will generally start to recover in six to nine months, and additional EMG testing can indicate if there are early signs of nerve regeneration.
- The acute pain associated with PTS can be treated with oral steroids, but it is frequently non-responsive to nonsteroidal anti-inflammatory drugs (NSAIDs).
- Patients are encouraged to return for periodic evaluations (every two to three months) to monitor their progress using EMG, physical examination, and imaging.
- Physical therapy may be helpful for patients to strengthen muscles once signs of nerve regeneration are seen.
Surgery may be considered for people who have prolonged symptoms, especially in those who do not show signs of improvement at around 9 to 12 months after symptoms first appear.

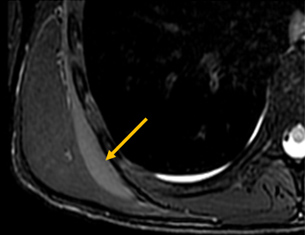
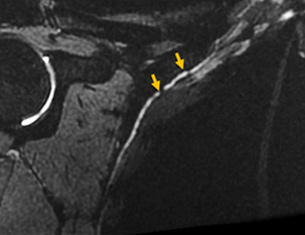
Atrophy of the brachialis muscle in the upper arm caused by muscle denervation secondary to neuropathy of the musculocutaneous nerve.
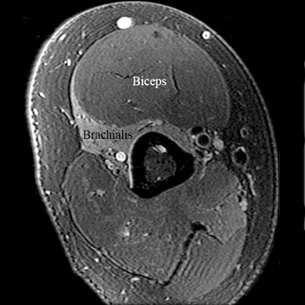
MR neurogram showing denervation of the brachialis muscle. The biceps muscle remains unaffected.
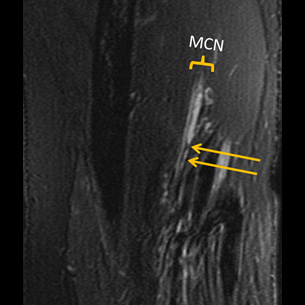
MR neurogram of musculocutaneous neuropathy with hourglass-like constrictions of the brachialis fascicular nerve bundle.
Parsonage-Turner syndrome webinar for patients
"Understanding Parsonage-Turner syndrome" by the HSS Peripheral Nerve Team.
HSS Parsonage-Turner syndrome research
Further research is needed to better understand the cause and possible treatments for PTS. At HSS, our dedicated team of physicians are currently conducting multiple research studies related to Parsonage-Turner syndrome. There are currently two studies open to enrollment:
- PTS Biomarkers Study: This NIH-funded study aims to determine whether MR neurography, ultrasound, and EMG are reliable markers of disease activity, muscle strength, and overall functional recovery. This study is open to enrollment to patients who have developed PTS symptoms in the past six months.
- PTS Registry: This is a survey-based study that is being conducted to understand the natural history of Parsonage-Turner syndrome from symptom onset to recovery. This study is open to enrollment to patients currently experiencing symptoms of Parsonage-Turner syndrome.
In addition to conducting the two current PTS studies, HSS physicians organize an international PTS-focused study group. Within the United States, the group comprises researchers from HSS, UCSF, and Beth Israel Deaconess (Boston). Internationally, the group includes members from Ente Ospedaliero Cantonale (Switzerland), Rabdboud University Medical Center & JBZ (Netherlands), and Semmelweis University (Hungary).
To learn more about our research studies, please email us at RadNerve@hss.edu.
Articles related to Parsonage-Turner syndrome
Updated: 11/29/2023
Reviewed and updated by Darryl B. Sneag, MD; Ek Tsoon Tan, PhD; Clare Nimura, BA
References
Krishnan KR, Sneag DB, Feinberg JH, Nwawka OK, Lee SK, Arányi Z, Wolfe SW. Outcomes of Microneurolysis of Hourglass Constrictions in Chronic Neuralgic Amyotrophy. J Hand Surg Am. 2021 Jan;46(1):43-53. doi: 10.1016/j.jhsa.2020.07.015. Epub 2020 Aug 28. PMID: 32868098.
Krishnan KR, Sneag DB, Feinberg JH, Wolfe SW. Anterior Interosseous Nerve Syndrome Reconsidered: A Critical Analysis Review. JBJS Rev. 2020 Sep;8(9):e2000011. doi: 10.2106/JBJS.RVW.20.00011. PMID: 32890049.
Krishnan KR, Wolfe SW, Feinberg JH, Nwawka OK, Sneag DB. Imaging and treatment of phrenic nerve hourglass-like constrictions in neuralgic amyotrophy. Muscle Nerve. 2020 Nov;62(5):E81-E82. doi: 10.1002/mus.27049. Epub 2020 Sep 14. PMID: 32841403.
Morena J, Tan ET, Campbell GJ, Bhatti P, Li Q, Geannette CS, Lin Y, Milani CJ, Sneag DB. MR Neurography and Quantitative Muscle MRI of Parsonage Turner Syndrome Involving the Long Thoracic Nerve. J Magn Reson Imaging. 2023 Sep 13. doi: 10.1002/jmri.29007. Epub ahead of print. PMID: 37702553.
Queler SC, Towbin AJ, Milani C, Whang J, Sneag DB. Parsonage-Turner Syndrome Following COVID-19 Vaccination: MR Neurography. Radiology. 2021 Aug 17:211374. doi: 10.1148/radiol.2021211374. Epub ahead of print. PMID: 34402669; PMCID: PMC8488809.
Sneag DB, Kiprovski K. MR Neurography of Bilateral Parsonage-Turner Syndrome. Radiology. 2021 Sep;300(3):515. doi: 10.1148/radiol.2021204688. Epub 2021 Jul 6. PMID: 34227884; PMCID: PMC8409009.
Sneag DB, Arányi Z, Zusstone EM, Feinberg JH, Queler SC, Nwawka OK, Lee SK, Wolfe SW. Fascicular constrictions above elbow typify anterior interosseous nerve syndrome. Muscle Nerve. 2020 Mar;61(3):301-310. doi: 10.1002/mus.26768. Epub 2019 Dec 13. PMID: 31773766.
Sneag DB, Rancy SK, Wolfe SW, Lee SC, Kalia V, Lee SK, Feinberg JH. Brachial plexitis or neuritis? MRI features of lesion distribution in Parsonage-Turner syndrome. Muscle Nerve. 2018 Sep;58(3):359-366. doi: 10.1002/mus.26108. Epub 2018 Mar 25. PMID: 29461642.
Sneag DB, Saltzman EB, Meister DW, Feinberg JH, Lee SK, Wolfe SW. MRI bullseye sign: An indicator of peripheral nerve constriction in parsonage-turner syndrome. Muscle Nerve. 2017 Jul;56(1):99-106. doi: 10.1002/mus.25480. Epub 2017 Mar 2. PMID: 27864992.
Sneag DB, Urban C, Li TY, Colucci PG, Pedrick EG, Nimura CA, Feinberg JH, Milani CJ, Tan ET. Hourglass-like constrictions on MRI are common in electromyography-confirmed cases of neuralgic amyotrophy (Parsonage-Turner syndrome): A tertiary referral center experience. Muscle Nerve. 2023 Aug 23. doi: 10.1002/mus.27961. Epub ahead of print. PMID: 37610034.
van Alfen N, van Eijk JJ, Ennik T, Flynn SO, Nobacht IE, Groothuis JT, Pillen S, van de Laar FA. Incidence of neuralgic amyotrophy (Parsonage Turner syndrome) in a primary care setting--a prospective cohort study. PLoS One. 2015 May 27;10(5):e0128361. doi: 10.1371/journal.pone.0128361. PMID: 26016482; PMCID: PMC4445915.
Van Eijk JJ, Groothuis JT, Van Alfen N. Neuralgic amyotrophy: An update on diagnosis, pathophysiology, and treatment. Muscle Nerve. 2016 Mar;53(3):337-50. doi: 10.1002/mus.25008. Epub 2016 Jan 20. PMID: 26662794.

