Laboratory for Joint Tissue Repair and Regeneration
Our laboratory investigates the basic cellular and molecular mechanisms of healing of joint tissues that are involved in common sports injuries, including tendon, ligament, meniscus, and cartilage. This research complements clinical practice, as injuries to these tissues are common, requiring surgical intervention for:
- tendon repair
- ligament reconstruction
- cartilage repair and transplantation
- meniscus repair and transplantation
A particular strength of the program is the close collaboration between clinician-scientists and a multidisciplinary team of investigators with expertise in cell biology, molecular biology, developmental biology, biomechanics and biomaterials, which informs research that has strong clinical relevance and that can ultimately be translated to clinical applications. As a clinician-scientist, my overall goal is to use our research findings to develop novel and innovative therapies for our patients.
Areas of Investigation
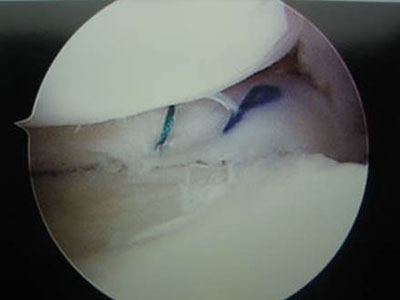
- The effect of joint motion and strain loading on anterior cruciate ligament graft healing
- Investigation of the role of tissue-specific activated endothelial cells on rotator cuff tendon healing and overuse tendonopathy
- The role of Indian hedgehog signaling in ACL graft healing and rotator cuff tendon repair
- Evaluation of novel materials for meniscus transplantation and replacement
- Development of a mouse model of supraspinatus tendon impingement and overuse tendinopathy
- Development of in vivo imaging techniques for small animals models, including fluorescent molecular imaging, multi-photon microscopy, and ultra-short TE MRI
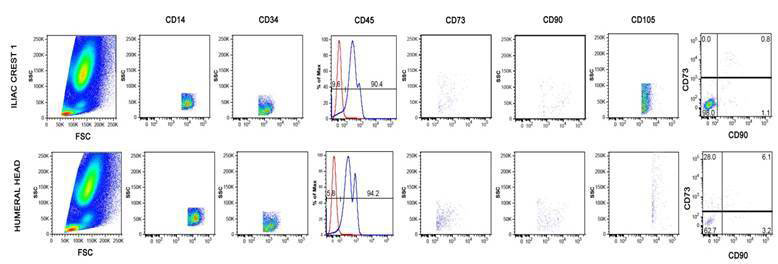
- Evaluation of stem cells derived from synovium, synovial fluid, and bone marrow for chondrogenesis
- Use of a murine model of post-traumatic arthritis to evaluate cell-based therapy and lubricin-mimetics
- Our murine models of rotator cuff tendon repair, ACL reconstruction, overuse tendonopathy, and post-traumatic arthritis now allow use of transgenic animals to examine the role of specific molecular factors in tissue healing and regeneration
Our overall focus relates to common soft tissue injuries seen in athletes and active individuals. Our laboratory investigates the basic cellular and molecular mechanisms of healing of joint tissues that are involved in common sports injuries, including tendon, ligament, meniscus, and cartilage. This research complements clinical practice, as injuries to these tissues are common, requiring surgical intervention for:
- tendon repair
- ligament reconstruction
- cartilage repair and transplantation
- meniscus repair and transplantation

A particular strength of the program is the close collaboration between clinician-scientists and a multidisciplinary team of investigators with expertise in cell biology, molecular biology, developmental biology, biomechanics and biomaterials, which informs research that has strong clinical relevance and that can ultimately be translated to clinical applications. As a clinician-scientist, my overall goal is to use our research findings to develop novel and innovative therapies for our patients.
Our laboratory consists of a multidisciplinary team of investigators with expertise in cell biology, molecular biology, developmental biology, biomechanics, mechanical engineering, and biomaterials, and orthopaedic surgeons from the Sports Medicine Service.
Principal Investigator
Scott A. Rodeo, MD, Co-Director, Tissue Engineering, Regeneration, and Repair Program
Laboratory Personnel
Xiang-hua Deng, MD, Senior Scientist:
Ying Liang (Lilly): Histology Technician
Camila B. Carballo, PT, PhD: Instructor
Alexander Piacentini, MS: Lab Manager
Wataru Morita, MD, PhD: Post-doctoral Fellow
Laura Moore, MD, PhD: Clinical Fellow
Claire Eliasberg, MD: Resident
Daniel Edon, MS: Research Coordinator
Samuel Green, Janice Havasy, Sarah Caughey, Edward Bowen, Nate Disser, Vincent Yao, Iryna Ivasyk, Leonardo Sanchez: Medical Students
HSS Collaborators
Suzanne Maher, PhD
Chitra Dahia, PhD
Matt Koff, PhD
Miguel Otero, PhD
Hollis Potter, MD
Lionel Ivashkiv, MD
Alessandra Pernis, MD
Kyung Park-Min, PhD
External Collaborators
Ansary Stem Cell Institute at Weill Cornell Medical College (Shahin Rafii, PhD and Dan Nolan, PhD)
Large animal surgery, Cornell University Veterinary Medical Center (Lisa Fortier, DVM, PhD)
Citigroup Biomedical Imaging Center, Weill Cornell Medical College (Jon Dyke, PhD and Doug Ballon, PhD)
Biomedical Engineering, Cornell University (Larry Bonassar, PhD)
Hazel Szeto, MD, PhD, Stealth Biotherapeutics and Weill Cornell Medical College
The New York Stem Cell Foundation Research Institute (Giuseppe de Peppo, PhD and Martina Sladkova, PhD)
Alumni
Katsunori Suzuki, MD, Oji General Hospital, Tomakomai, Japan
Kouji Suzuki, MD, Sapporo, Japan
Sumito Kawamura, MD, Kobayashi Hospital
Kazutaka Izawa, MD, Toneyama National Hospital, Osaka, Japan
Hyon Jeong Kim, MD, PhD, Seoul, Korea
Aruna Seneviratne, MD, Lenox Hill Hospital, New York
Asheesh Bedi, MD, University of Michigan
Robert Brophy, MD, Washington University, St. Louis
Richard Ma, MD, University of Missouri
Peyton Hayes, MD, ProHEALTH Care Associates, Long Island, New York
Jonathan Packer, MD, University of Maryland
Clifford Voigt, MD, Lenox Hill Hospital, New York
Mark Stasiak, MEng, City College of New York
Andrew Carbone, MD, New York Medical College
Michael Schaer, MD, University Hospital of Bern, Switzerland
Guang-Ting Cong, MD, Mount Sinai Hospital, New York
Amir Lebaschi, MD, University of Connecticut
Christopher Camp, MD, Mayo Clinic, MN
Dean Wang, MD, University of California Irvine Medical Center
Yusuke Nakagawa, MD, PhD, Tokyo Medical and Dental University, Japan
Susumu Wada, MD, PhD, St. Luke’s International Hospital, Tokyo, Japan
Zoe Album, BS, Facebook, NY
Arielle Hall, BS, Rowan University School of Osteophatic, New Jersey
Daniel Nemirov, BS, Jefferson Medical College, PA
Brett Croen, BS, Drexel University College of Medicine, PA
Tyler Uppstrom, MD, Hospital for Special Surgery, NY
Xueying Zhang, MD, PhD, Shanghai 6th People's hospital, China
Opportunities to join our group
We have opportunities for medical students, residents, fellows, and post-doctoral candidates to work in our laboratory. Our laboratory carries out translational related to repair of tendon, ligament, meniscus, and articular cartilage. Medical students, residents, and fellows can assist with animal surgery, tissue dissection, tissue preparation for histology and biomechanics, histologic analysis, and biomechanical testing. Education in basic laboratory techniques and methodologies for tissue analysis is an important component of our activities.
We run a robust summer medical student research program, and we also participate in the Cornell University Department of Biomedical Engineering summer student immersion program
Recent Publications
- Wang H, Koff MF, Potter HG, Warren RF, Rodeo SA, Maher SA. An MRI-compatible loading device to assess knee joint cartilage deformation: Effect of preloading and inter-test repeatability. J Biomech. 2015 Sep 18;48(12):2934-40. doi: 10.1016/j.jbiomech.2015.08.006. Epub 2015 Aug 13.
- Ma R, Ju X, Deng X, Rodeo S. A novel small animal model of differential anterior cruciate ligament reconstruction graft strain. Journal of Knee Surgery 2015; 28: 489-495.
- Rodeo SA, Voigt C, Ma R, Solic J, Stasiak M, Ju X, El-Amin S, Deng X. Use of a new model allowing controlled uniaxial loading to evaluate tendon healing in a bone tunnel. In press, Journal of Orthopaedic Research, 2015.
- Carbone A, Carballo C, Ma R, Wang H, Deng X, Dahia C, Rodeo S. Indian hedgehog signaling and the role of graft tension in tendon-to-bone healing: Evaluation in a rat ACL reconstruction model. J Orthop Res. 2015 Oct 8. doi: 10.1002/jor.23066.
- Rodeo SA, Lebaschi A, Carballo C, Zong J, Khilnani T, Cunningham M, Lane J, Maher S. Specialty Update: What's New in Orthopaedic Research 2015. J Bone Joint Surg Am. 2015 Dec 2;97(23):1972-8. doi: 10.2106/JBJS.O.00958.
- Atesok K, Fu F, Sekiya I, Stolzing A, Ochi M, Rodeo SA. Stem cells in degenerative orthopaedic pathologies: effects of aging on therapeutic potential. Knee Surg Sports Traumatol Arthroscopy, DOI 10.1007/s00167-015-3763-9.
- Sneag DB, Shah P, Koff MF, Lim WY, Rodeo SA, Potter HG. Quantitative Ultrashort Echo Time Magnetic Resonance Imaging Evaluation of Postoperative Menisci: a Pilot Study. HSS J. 2015 Jul;11(2):123-9. doi: 10.1007/s11420-014-9420-x. Epub 2014 Nov 18.
- Galatz LM, Gerstenfeld L, Heber-Katz E, Rodeo SA. Tendon regeneration and scar formation: The concept of scarless healing. J Orthop Res. 2015 Jun;33(6):823-31. doi: 10.1002/jor.22853. Epub 2015 Apr 27.
- Weber AE, Delos D, Oltean HN, Vadasdi K, Cavanaugh J,Potter HG, and Rodeo SA. Tibial and femoral tunnel changes after ACL reconstruction: A prospective 2-year longitudinal MRI study. American J. Sports Medicine 2015; 43:1147-1156.
- Kovacevic D, Gulotta LV, Ying L, Ehteshami JR, Deng XH, Rodeo SA. rhPDGF-BB Promotes early healing in a rat rotator cuff repair model. Clin Orthop Relat Res. 2015 May;473(5):1644-54. doi: 10.1007/s11999-014-4020-0.
- Mosca M and Rodeo S. Platelet-Rich Plasma for Muscle Injuries: Game Over or Time Out? Current Reviews in Musculoskeletal Medicine. DOI: 10.1007/s12178-015-9259-x.
- Hutchinson ID, Rodeo SA, Perrone GS, Murray MM. Can platelet-rich plasma enhance anterior cruciate ligament and meniscal repair? J Knee Surg 2015; 28:19–28.
Patents
- Method for Healing and Repair of Connective Tissue Attachment, U.S. PO: #6187742
- Instrumented boot for quantifying intra-operative joint contact mechanics (pending)
Funding Sources
- American Orthopedic Society for Sports Medicine
- Virginia Toulmin Foundation
- Arthroscopy Association of North America
- Orthopedic Research and Education Foundation
- Steven Tisch Foundation
- Charles Koch Foundation