Joint Replacement: Implant Bearing Surface Materials

Total joint replacement (also known as total joint arthroplasty) is regarded as among the most valued developments in the history of orthopedics. The procedure relieves pain and restores function to patients whose joints have been destroyed by trauma or disease. Although natural, human articular cartilage is the best bearing surface for joints, when there is too much damage to these tissues, man-made joint replacements are required. However, the higher level of friction in man-made implants compared to a person's natural bearings means that wear becomes an ongoing concern for joint replacement patients.
This article covers the following aspects of joint implant materials:
- Why are there so many different types of joint implants?
- Are modern implants safe?
- How are joint implants tested?
- What are the different types of joint implants?
- The future of joint replacement
- Is there one type of joint implant that fits best?
Why are there so many different types of joint implants?
The ongoing problem of wear in joint replacement implants has led to the reintroduction of many alternative bearing combinations.
Compared to healthy, organic cartilage surfaces, which have a surface friction of nearly zero, the friction between these man-made bearing surfaces is hundreds of times higher. This friction subjects the implant components to wear that can limit the longevity of the joint replacement and induce inflammatory responses in the tissues surrounding the joint itself.
For this reason, producing a low-friction bearing is fundamental to replacing damaged joint surfaces with implants fabricated from man-made materials. This will hopefully eliminate the need for an additional revision surgery by minimizing:
- surface wear
- inflammation in surrounding tissues
- the risk of eventual loosening of the implant
Results of friction and wear
Clinically speaking, friction and wear lead to the release of very small particles (typically less than 4/100,000 of an inch, or about 200 times smaller than a grain of sand) into the surrounding joint cavity. This initiates an aggressive inflammatory response.
The body mounts a cellular reaction to try to deal with the wear debris. This reaction, unfortunately, often leads to unwanted destruction of bone (called osteolysis) around the implant. When osteolysis becomes severe, it can cause pain, loosening of the implant and the need for revision surgery to replace the implant components. One way to relieve the problem of osteolysis and increase the longevity of joint replacements is to improve the wear resistance of the bearing materials.
Younger patients needing joint replacement
As younger and more active patients are seeking and receiving joint replacements, the importance of developing new materials to combat wear also increases. At HSS, the age at which patients undergo knee replacement surgery is rapidly decreasing (see Fig. 1). This change in the demographics of patients seeking knee replacement is the primary motivation for improving implant materials.
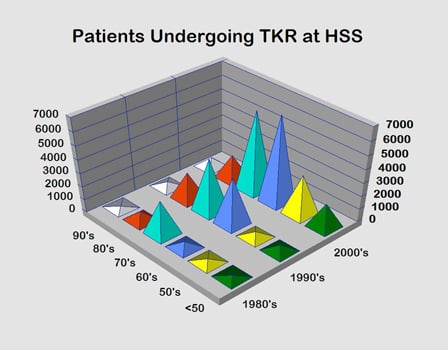
Figure. 1. Patients undergoing total knee replacement surgery at HSS
Are modern joint implants safe?
All the materials currently in use in joint replacement are considered safe from a medical standpoint. They are highly biocompatible, meaning that they cause little if any detrimental local or systemic problems due to an immune response or an allergic reaction.
Nonetheless, as total joint replacements remain in service for long periods of time, concern remains that adverse tissue responses may arise as a result of the continual release of wear particles from the prosthetic materials. (Find a knee replacement surgeon at HSS to suit your specific condition, location and insurance.)
How are joint implants tested?
Determining whether new types of implant bearing surfaces effectively reduce wear versus the conventional metal-on-polyethylene bearings is not as easy as it may seem. We are limited in our ability to study wear in the laboratory by our inability to simulate the lubrication conditions, the loads and the motions that occur over a broad range of daily activities by our patients.
Joint simulators are currently the best tools for studying wear because they provide an effective means of screening whether or not one combination of bearing surfaces is better than another. No acceptable animal models exist, and computer analyses of implant wear have only been proven to be effective for simpler constructs, such as ball-in-socket implants for the hip.
Complicating the problem further is that wear mechanisms differ depending on the joint. For this reason, data collected on a hip simulator may have little relevance for wear in a knee, elbow or shoulder replacement. Furthermore, the question is not just one of reducing the amount of wear, but also of the ways in which the size, shape and surface chemistry of released wear particles differ among various bearing surface combinations. These factors may ultimately influence the biological reaction and subsequent tendency for osteolysis.
Ultimately, the effectiveness of these surfaces can only be proven based on clinical results from prospective, randomized studies of total joint patients who have received either conventional or new bearing combinations. Some of these data have already started to emerge, so reviewing the current laboratory and clinical data for each of the new bearing surfaces is essential (read below).
What are the different types of joint implants?
There are three main types of joint implant materials, and they each have their advantages and disadvantages:
In the 1960s and 1970s, several materials were tried as bearing surfaces in joint arthroplasty, including Teflon® and metallic alloys such as stainless steel and cobalt-chromium alloy. But through the 1980s and much of the 1990s, the preferred combination was ultra-high-molecular-weight polyethylene bearing against cobalt-chromium.
Polyethylene results in a low coefficient of friction when bearing against a highly polished metallic or ceramic surface. Today, metal-on-polyethylene and ceramic-on-polyethylene combinations are considered as primary choices for bearing surfaces. However, ceramic-on-ceramic are also considered, as are metal-on-metal bearings in hip resurfacing surgeries.
Metal-on-metal bearings
Early problems
Metal-on-metal bearings were among the first to be used in total hip arthroplasty and found clinical success in the 1960s and 1970s. Metal-on-metal hip joints fell out of favor by most orthopaedic surgeons once the clinical results with metal-on-polyethylene joints proved superior.
However, failures during this earlier time period were likely due to poor metallurgy, poor manufacturing techniques and inferior implant designs. The casting process used to make metallic implants suffered from poor quality control. This sometimes restulted in products that had inferior wear resistance and which were prone to fracture in the body. Early metal-on-metal designs also often had small head-to-neck ratios. For this reason, it was common to experience impingement between the neck of the artificial femoral component and the rim of the artificial acetabulum. This impingement creates additional wear and can knock the acetabular component loose from the surrounding bone.
Benefits of the improved modern version
Improved metallurgy and manufacturing techniques led to resurgence in the use of metal-on-metal bearings for hip replacement. Cobalt-chromium alloys with well-controlled grain sizes and finely distributed carbides provide superior hardness and wear resistance compared to earlier versions of the alloy and to stainless steel and titanium alloy.
Clearance and conformity between the bearing surfaces and a smooth surface finish on the metallic bearings are now recognized as important factors that must be controlled as part of the design and manufacturing processes. Laboratory evidence from hip joint simulator studies has confirmed that these bearing surfaces can provide low wear joint implants. The strength of cobalt-chromium alloys in comparison to polyethylene and their increased toughness over ceramics provide additional benefits from the standpoint of hip implant design.
For example, the surface thickness of a one-piece metallic acetabular component can be smaller than modular components made from polyethylene and metal or from ceramic and metal, so larger femoral head sizes can be incorporated, providing an advantage in cases where joint stability is an issue. Similarly, the ability to manufacture large metallic shells allows for surface replacement of the hip joint, a bone-conserving operation geared toward young, active patients with good bone stock in the femoral head and neck.
Metal degradation concerns
Concerns with metal-on-metal bearing in total hip replacement continue to exist because clinical studies show that the release of ionic debris in metal-on-metal combinations is considerably higher than with other bearing combinations. Metal ions are transported to distant locations in the body, and elevated levels of metals have been found in serum and urine from patients with metal-on-metal hip replacements. In rare cases, the systemic levels have been associated with cobalt toxicity.
Several factors can influence metal levels in such cases, including the diameter of the joint. For example, resurfacing of the hip is intended to be bone-conserving by employing a large metallic cap secured to the head of the femur and a matching large metallic shell in the acetabulum. But as the size of the head increases, so does the amount of wear; indeed, metal-on-metal resurfacing patients have a significantly greater increase in serum chromium and cobalt levels than patients with a conventional total hip with a much smaller diameter metal-on-metal bearing.
Metal-on-metal bearings are not recommended for patients with poorly functioning kidneys because metal ions that would otherwise be excreted through the kidneys can build up in the blood. Also, though being a pregnant woman or a woman of child-bearing age is not necessarily a contraindication for metal-on-metal bearings, studies continue regarding metal ions crossing the placenta.
Clinical evidence is mounting that osteolysis and implant loosening in total hip patients with metal-on-metal bearings may be associated with hypersensitivity to metallic debris, but the direct scientific link between hypersensitivity and loosening remains to be found. Hypersensitivity has not been a significant problem for implants employing metal-on-plastic bearings, so the assumption is that the increased metal burden caused by both bearings being metallic may be responsible for these hypersensitivity reactions but not a direct cause of loosening.
Metal-on-metal bearings have not been applied to many joints other than the hip. Most other joints require different designs to provide adequate function, and therefore suffer from additional wear mechanisms for which metal-on-metal surfaces have few advantages.
“There is no universal agreement by surgeons on the precise indication for metal on metal bearings,” says Steven B. Haas, MD, Chief of the Knee Service at HSS, “but most surgeons agree that younger patients are the best candidates.”
Hip surfacing preserves more bone in the patient than conventional hip replacement. This has the potential of being a first-line treatment of painful, disabling arthritis in younger, active patients. If revision surgery is needed, the preservation of bone is an advantage in converting to a full hip replacement device. However, long-term results using current technology in the US are not yet available. Prospective outcome research on hip surface replacement is currently being performed at HSS, which will further define the role of surface replacement surgery.
Metal-on-polyethylene bearings
One of the most used bearing surface combinations for joint replacement is metal on polyethylene, a form of plastic that provides marked durability. The two groups most traditionally considered for this material are:
- older adults in their seventies or eighties who are relatively sedentary
- younger, active patients who may subject their joints to activities involving repetitive impact
From a clinical perspective, metal on polyethylene has the longest-term data available for hip replacement. There will be some degree of measurable wear, but the effects of wear degradation related to metal on polyethylene, more often than not, are local phenomena that can readily be followed radiographically.
The goal of finding new means of reducing wear degradation in polyethylene has lead to some interesting developments in this material in the last two decades.
Ultra-high molecular weight polyethylene bearings
A substantial leap forward was made with the discovery in the late 1980s of the role of oxidation in the wear performance of polyethylene.
The adverse effects of oxidation during radiation sterilization
Polyethylene components, like most medical devices, are most often sterilized by exposure to gamma radiation. Unfortunately, the radiation, while penetrating through the component, has enough energy to break the chains that form the molecular backbone of the polymer. If the radiation exposure is performed while the component is exposed to air, the broken ends can react with oxygen, causing harmful changes, including a decrease in molecular weight, a dramatic loss of ductility, and a decrease in strength. The combined effect makes the polyethylene markedly more susceptible to wear.
Sterilization options
One important form of alternative bearing surface has emerged simply by removing the chance that the polyethylene can oxidize during the sterilization process. Device manufacturers have accomplished this task in two ways:
- Placing polyethylene joint replacement components into sealed packages that contain either a vacuum or an inert gas, such as nitrogen or argon, instead of air.
- Replacing radiation altogether, instead exposing polyethylene components to ethylene oxide or gas plasma, neither of which imparts enough energy to cause oxidation.
Though these alterations in sterilization can eliminate degradation, they do not all have the same beneficial impact on wear. Techniques that eliminate irradiation altogether also eliminate the benefit of the additional cross-linking between the molecular chains in the polymer that occurs with gamma radiation. Indeed, clinical results show increased rather than decreased wear in hip replacements employing polyethylene components sterilized by exposure to ethylene oxide rather than irradiation.
Increased cross-linking: Advantages and possible disadvantages
Perhaps the most significant alteration in modern polyethylene joint replacement components is the inclusion of elevated levels of radiation, beyond those required to simply sterilize the implant. The goal is to induce even higher levels of cross-linking than occur with the conventional sterilization dose. Significantly reduced wear is the primary advantage of elevated cross-linking. Highly cross-linked polyethylenes have been in clinical use since about the turn of the millennium, and results show dramatic decreases in wear in total hip replacements over those seen with conventional polyethylene.
This increased wear resistance has also renewed interest in larger femoral heads as a means of reducing the risk of dislocation. With a larger head size, sliding distance between the bearing surfaces is increased and the resulting amount of wear is high, so conventional metal-on-polyethylene bearings were typically small in diameter (32 mm or less). So, the improvement in wear resistance allows surgeons to also implant hip replacements with inherently better stability.
The changes in mechanical properties that accompany increased cross-linking may pose the biggest threat to the clinical effectiveness of these materials. Increased cross-linking, while decreasing wear, makes the material more brittle. The use of this material in knee replacement is limited. “There are little clinical data on the use of highly cross-linked polyethylenes in knee replacement, and some of the laboratory data raise concern,” notes Dr. Haas. Indeed, the types of motion and wear that occur in knee replacement could lead to fracture or other failure of the highly cross-linked polyethylenes in knees.
This is not to say that polyethylene degradation is a thing of the past. Highly cross-linked polyethylene components examined after being retrieved from patients at revision surgeries have shown continued degradation, but at rates much lower than those seen with the conventional polyethylene irradiated in air back in the twentieth century. To minimize the chance that such degradation would be a long-term problem, even newer forms of hihly cross-linked polyethylenes containing antioxidants like vitamin E have been introduced. Those these materials have not shown a further improvement in wear above that of highly cross-linked polyethylenes without antioxidants, they have shown increased resistance to degradation.
Ceramic bearings
Advantages
Fully dense ceramics, alumina and zirconia, are used in total joint replacements specifically for the purpose of providing more wear resistant bearing surfaces; they have few other mechanical advantages over metallic alloys. Because of their hardness, ceramics can be polished to a very smooth finish and remain relatively scratch resistant while in use as a bearing surface.
Disadvantages
The most significant disadvantage of ceramics is their brittle nature, making them susceptible to fracture. As with the case of metal-on-metal bearings, where improvements in metallurgy have sparked renewed interest, improvements in ceramic quality have led to increased interest in ceramic bearings. Increased chemical purity and reduced grain size have lead to increased strength and a dramatic reduction in the number of fractures seen clinically. Nonetheless, strength and toughness remain issues, particularly in acetabular components of ceramic-on-ceramic hip replacements, where impingement of the femoral and acetabular components at extreme ranges of motion can lead to fracture.
Most patients whose active lifestyles subject them to repetitive impact are not good candidates for ceramic bearings. For example, patients in their fifties who are looking to remain actively engaged in less rigorous sports such as golf are typically a good fit for this type of implant.
Types of ceramic bearing materials
Two types of ceramic bearing materials are commonly used: a zirconia-toughened alumina and an oxidized zirconium material. The latter material is made by ceramizing a zirconium metallic alloy so that the surface layer, forming the bearing surface for the femoral head of a total hip replacement, transfroms into zirconia ceramic.
Zirconia-toughened alumina-on-polyethylene
Long-term experience with alumina ceramic-on-conventional polyethylene bearings for hip replacement showed reduced wear rates over those typically seen with metal-on-conventional polyethylene bearings, with an associated decrease in osteolysis. The newer zirconia-toughened alumina bearing against highly cross-linked polyethyene has shown wear rates comparable to that of metal-on-highly cross-linked polyethylene bearings. Concern that the zirconia in these materials would undergo a harmful transformation into a less suitable crystalline phase, thus increasing wear and decreasing strength, has not been borne out by measurements on retrieved components removed from patients at revision surgeries and on artificially aged laboratory specimens. Thus, zirconia-toughened ceramic has become a viable bearing material for hip replacement.
Alumina-on-alumina
Alumina-on-alumina total hip replacements have been used more extensively in Europe than in the United States.
In general, alumina-on-alumina joints have shown very low wear rates clinically, though the results are design dependent. Recent reports also show excellent wear resistance in young patients, with no measurable wear and no evidence of osteolysis even beyond a decade of follow-up. Furthermore, very few implant fractures have been observed, even in this high demand patient population, lending further credence to the improved mechanical properties of alumina.
One unusual issue affects a small number of patients who have alumina-on-alumina bearings: reports of an audible squeaking sound during normal ranges of motion after surgery. Studies have shown that 1-10% of these patients may experience this problem. While ceramic bearings have been used extensively in hips, the use of ceramic bearings in other joint replacements is much more limited. For joint designs such as knee replacements that require bearings with nonconforming surface shapes to provide the patient with adequate function, the advantages of ceramic-on-ceramic bearings are unclear.
Alumina-on-alumina bearings for knee replacement have been used primarily in Japan. Evidence for the effectiveness of these bearings is very limited, given the short length of follow-up, the lack of comparative data for other bearing surfaces in the same design, and patient selection (for example, one study was limited to only rheumatoid arthritis patients).
Oxinium (oxidized zirconium) on polyethylene
Oxidized zirconium,known as Oxinium (which is a brand name applied by orthopedic device manufacturer Smith & Nephew), is a metal-ceramic hybrid technology. Zirconium alloy, a metal, is treated with high pressure and heat in the presence of oxygen; this process converts the metallic surface of the implant to a ceramic. This leads to an implant that has surface properties of ceramic, which is harder, smoother, and has less friction than the metal.
Oxinium is used for femoral heads in hip replacement and the femoral component in knee replacement. Although clinical experience has been promising, further testing is necessary. The clinical data thus far on implant survival and wear in knee replacement have been positive, but longer term studies will be needed to prove that the improved bearing properties of oxidized zirconium lead to longer lasting implants.”
The future of joint replacement
"The final frontier in man-made joint replacement is the longevity of the implant, to prevent the problem of osteolysis,” explains Edwin P. Su, MD. “The alternate bearings are an attempt to bring it to the next level and get a further increase in longevity by decreasing the wear degradation problems.”
The future of joint replacement may see the implementation of other intriguing surface materials. Surfaces made of diamond have been produced recently, and there is much discussion of the promise of hardened titanium, due to its smooth exterior.
Is there one type of joint implant that fits best?
Is there one "best bearing" combination that fits all joints in all patients? Probably not. Most joint replacement surgeons will use all types of surfaces, recognizing that there are advantages and disadvantages. "At the end of the day, we have to customize what we do for patients on an individual basis” says Dr. Padgett. The age of the patient, the patient’s expected activity levels, and the extent of the patient’s joint problems are among a long list of factors that the surgeon must consider in choosing an implant. And despite the concern over wear and osteolysis, it must be remembered that joint replacement is a highly successful treatment with few complications.
Perhaps one set of bearing materials will eventually emerge as the best for each joint in the body. That will depend on clinical experience as well as continuing research and development to understand the biological consequences of wear and to adopt further improvements in materials as they become available. For now, the decrease in wear afforded by the new bearing surfaces represents an impressive milestone in the further improvement of total joint replacement.