Arthritis of the Shoulder
After the hip and knee, the shoulder is the third most common joint affected by arthritis, perhaps because in most people, it is not a weightbearing joint, as are the large joints of the lower limbs. However, as in the hip and knee, the loss of cartilage that characterizes shoulder arthritis is frequently a source of severe pain, limited function, joint stiffness, and significant diminishment of quality of life. While there is no cure for arthritis, there are many treatments, both nonsurgical and surgical, that enable the symptoms to be well treated and for patients to maintain active lifestyles.
Arthritis has its word origin from the Greek word, "arthron," meaning joint. "Itis" probably of Latin derivation, and refers to inflammation. While literally arthritis therefore means “inflamed joint,” it has come to refer to any condition of the joint in which there is damage to the smooth cartilage covering a moving surface of a joint (called the articular cartilage), eventually leading to cartilage loss, in the end stage resulting in "bone on bone" of the joint surfaces, and pain.
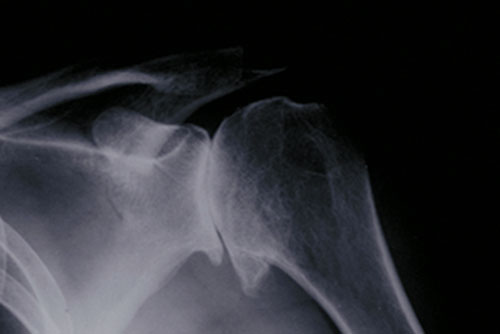
Fig. 1: X-ray showing osteoarthritis of the shoulder joint
The normal, unaffected shoulder
The shoulder is made up of a number or interconnected bones. The upper end of the humerus is a ball, called the humeral head, which “rests against” the socket, a part of the scapula called the glenoid. Unlike the hip, also a ball-socket joint but one with a deep socket made for stability, the shoulder is made not for stability but motion - and has the most motion of any joint in the body. The ball of the shoulder joint moves against the socket, but because it “rests against” the socket, rather than being well contained in it, it is reliant on the soft tissues for both its stability and motion. It is stabilized by both ligaments (cords that attach to both ball and socket) and tendons (soft tissue attachments of muscle to bone). The tendons of the shoulder “rotate” the ball in the socket, and are called the rotator cuff. The four rotator cuff tendons thus supply movement to the shoulder and stability, and can themselves be subject to injury, wear and tear, and degeneration (rotator cuff tear).
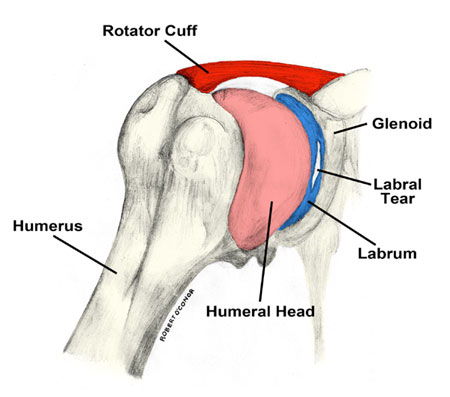
Fig. 2: Anatomy of the shoulder, featuring the humerus (upper arm bone), the glenoid (shoulder socket), the ligaments, and tendons. [Illustration by Robert O'Conor]
What kinds of arthritis affect the shoulder?
The most frequently occurring types of arthritis which affects the shoulder are osteoarthritis, inflammatory arthritis, rotator cuff tear arthropathy, osteonecrosis and post-traumatic arthritis.
Osteoarthritis: Similar to the hip and knee, this is also called a “wear and tear” type of arthritis, and probably occurs as some combination of use, genetics, micro trauma, and increased forces across the joint. The cartilage loses its normal chemical makeup, becomes frayed and worn, and eventually disappears; without this protective covering, the underlying bones grind against one another, causing pain.
Inflammatory arthritis: In conditions such as Rheumatoid Arthritis, multiple factors often having to do with the immune system, lead to inflammation of the joint and joint lining, ultimately wearing away the cartilage surfaces. Fortunately, the medical treatment of many types of inflammatory arthritis has made tremendous advances, and the need for surgical treatment has greatly diminished.
Rotator cuff tear arthropathy: This is the end stage of very large tears of the rotator cuff tendon. A confluence of four muscles which stabilize and are the primary movers of the shoulder joint, which have been left untreated. While large tears of the rotator cuff tendon, are uncommon, an estimated 4% of patients with untreated rotator cuff tears develop cuff tear arthropathy. Treatment of shoulder arthritis caused by cuff tear arthropathy can be particularly difficult, since it results from damage to both soft tissue support of the joint as well as the joint surface.

Fig. 3: Xray showing both arthritis and big tear of rotator cuff tendon
Osteonecrosis (Avascular necrosis): An unusual condition in which the blood supply to the bone forming the ball of the shoulder is interrupted, leading to the death and collapse of a segment of the bone. With loss of the bone support, the overlying cartilage is subject to forces which cause the cartilage to become damaged as well.
Post-Traumatic Arthritis: This can result from a fracture of the ball or of the socket, in which the cartilage surface is damaged at the time of the bone fracture. Eventually, this damage can cause the cartilage surface to wear out and disappear. (Learn more in What Is Post Traumatic Arthritis? Exercises, Causes and More.)
What are the symptoms of shoulder arthritis?
As with other joints, the most common symptom of shoulder arthritis is pain during activity. In time, should pain can occur at rest, and may even interrupt sleep. As the cartilage disappears, the joint becomes stiff, reducing range of motion, and limiting activity, often causing interference with even the most common tasks of everyday life, such as dressing, reaching for objects, and even personal hygiene. As joint motion is lost, tasks such as driving, athletic activity, housework, and even writing and computer work can be affected. The pain is frequently centered on the back of the shoulder, but commonly is felt all the way down the arm to the elbow.
Perhaps the most disabling symptom for most people is the loss of sleep, as it frequently becomes difficult to find a comfortable position either on the affected or unaffected side.
Motion is often severely affected, and may be accompanied by cracking, grinding, or catching (crepitus) as the ball/socket bones rub against one another.
The doctor's evaluation
With progression of shoulder arthritis symptoms, examination will frequently demonstrate stiffness or loss of motion. Strength may be affected, and crepitus elicited as the arm is moved.
Usually an X-ray will show the degree of articular cartilage loss and the presence of arthritis. Since cartilage does not show on an X-ray, in a normal joint its presence is demonstrated by a “space” between ball and socket. As the cartilage disappears, the space narrows on an X-ray, and in the end stage, the bone of the ball can be seen directly against the bone of the socket. In addition, bone spurs (osteophytes) which develop around the joint margins are frequently seen in some types of arthritis.
A CT scan is a computerized study which may be used to outline the bone of the shoulder joint in more detail, while a MRI scan is a test in which a magnetic coil is put over the area to be studied. This gives information about the bone and cartilage, but has its greatest use in demonstrating the condition of the surrounding soft tissues, particularly the muscles and tendons of the shoulder.
How is shoulder arthritis treated?
As is the case in any other joint, the initial treatment of shoulder arthritis is usually nonsurgical. This may include: activity modification, physical therapy and other measures. If these prove insufficient, arthroscopic surgery or shoulder replacement may be appropriate. If a person with severe shoulder arthritis has also had a prior rotator cuff tear, they may need a special surgery known as a reverse shoulder replacement.
Activity modification: avoiding the activities which put the most stress on the arms, reducing the weight lifted by the involved arm, and attempting to modify athletic activities to those which may put less stress on the involved arm.
Moist heat may make the arm feel more comfortable.
Icing the shoulder three or four times daily may help role reduce inflammation, particularly after sports or stress on the shoulder
Physical therapy: may play a role in maintaining or improving range of motion and strength, but may in some circumstances aggravate the pain from arthritis – so its role should be reevaluated if it is a source of aggravation of pain.
Nonsteroidal ant-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, or aspirin can be effective over-the-counter medication. These medications can irritate the stomach, and most people should take them with meals. Prescription anti-inflammatory medications are also available, and may be more convenient in dosages require, have fewer side effects, and be better tolerated. In any event, your doctor should be made aware of any medications you may be taking, and the role of potential interactions.
Dietary supplements, such as glucosamine or chondroitin sulfate. While some patients find relief with these, there is little scientific evidence of the role or value of dietary supplements in arthritis treatment. In addition, the FDA does not regulate these supplements, and there may be interactions with other medications you are taking. Consultation with your physician is recommended before taking dietary supplements.
A cortisone injection may help a role to treat the inflammation inside the joint. While there is often little risk associated with a joint injection of cortisone, its effects, if positive, may not be long lasting. In addition, patients who have diabetes may see a rise in blood sugar for a variable period of time after a cortisone injection
Injection of viscosupplementation: These synthetic compounds such as hyaluronic acid and derivatives are similar in structure to normal joint fluid. They are injected into the joint in an effort to increase lubrication of the joint. These compounds are expensive and are approved only for use in the knee, the joint in which the most medical experience has been obtained. There is little information about whether there is any role for these compounds in the treatment of shoulder arthritis.
What is the surgery for shoulder arthritis?
If non-operative treatments are not effective, your doctor may discuss either shoulder arthroscopy or shoulder replacement surgery.
Arthroscopy: this is a minimally invasive operation requiring anesthesia, in which a small camera is placed inside the joint through a small incision. Through another incision, small instruments can be brought inside the joint to manipulate tissue.
Arthroscopy of the shoulder to remove loose fragments of cartilage and bone in the joint (debridement) may play a role in early arthritis when there is little damage to the joint surface. This does not eliminate arthritis, but can be helpful in removing loose pieces of tissue which are irritants. The benefits may be minimal, subjecting the patient to an operation and anesthesia, with essentially no role in effectively treating the symptoms when arthritis is advanced.
Shoulder replacement – A shoulder replacement is an operation similar in concept to hip replacement or knee replacement, in which implants made of plastic and metal are placed to create new joint surfaces. During this operation, which requires an incision as with all open surgery, the arthritic ball is removed and replaced by a metal ball (prosthesis) that attaches to a metal stem that goes inside the upper humerus bone (similar to the way in which ice cream sits on top of a cone). The arthritic socket is covered by a smooth plastic socket, also called a prosthesis. It is the smooth metal ball moving on the smooth plastic socket that relieves pain.
Rehabilitation after surgery
Because the shoulder has the widest range of motion of any joint in the body, recovery from injury, damage, or surgery is frequently aided by rehabilitation and physical therapy, either to improve or maintain motion, or to foster improvements in strength.
Future developments
As in all areas of orthopedic surgery, the future continues to be bright for treatment options in shoulder arthritis. At HSS, considerable time and effort is dedicated to improving outcomes and treatment methods to offer our patients with arthritis. Areas currently being investigated include:
- attempting to understand why arthritis develops in an effort to apply our knowledge to its prevention
- new medications by mouth – or other means of administration – to treat the varied arthritic conditions
- joint lubricants, similar to those used in the knee, are being studied
- joint replacement surgery, including ongoing investigation of designs and materials, and understanding how these can be improved
- biologic materials to restore articular cartilage surfaces on a joint or to encourage or engineer more normal tissue when the joint is damaged, to foster new growth and promote healing
Summary
While less common than hip or knee arthritis, shoulder joint arthritis can be equally disabling and have a significant impact on quality of life.
Fortunately there are both effective non-operative and operative treatments, depending on the severity and degree of disability, which makes this disease one which is compatible with a productive, healthy, active life.
Articles on Treatments for Shoulder Arthritis

