Patellofemoral Joint Replacement
Patellofemoral joint replacement, a type of partial knee replacement (also known as unicompartmental knee replacement), is a surgical treatment option for individuals with knee arthritis that is confined to the patellofemoral compartment anterior aspect of the knee.
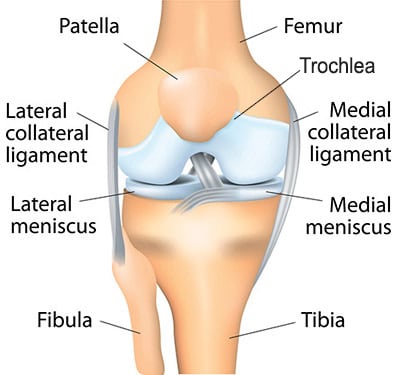
Anatomy of the Patellofemoral Joint
Patellofemoral arthritis is diagnosed when there is significant loss of cartilage from the joint surface of the patella and the trochlea, the groove on the femur in which the patella glides as the knee is flexed or extended. Underlying causes of patellofemoral arthritis include patellar instability; a severe injury to the patella such as a fracture; mal-alignment, in which there is an increased load on the patella and early wear of the cartilage; and osteoarthritis that does not have a specific origin.
In contrast to total knee replacement—in which all three compartments of the knee (femur, tibia, and patella) are replaced with a prosthesis—patellofemoral joint replacement is a less invasive surgery that involves resurfacing the back of the kneecap and the front of the thighbone. Although the surgery was first introduced in the 1970s, early designs were not ideal. In the last decade, however, newer designs and materials have made patellofemoral joint replacement as predictable in the treatment of patellofemoral arthritis as total knee replacement is for patients with generalized arthritis of the knee.
Diagnosis and Treatment
Diagnosis of patellofemoral arthritis is based on a physical examination, patient history and imaging. Typically, patients with patellofemoral arthritis have isolated pain in the front of the knee associated with prolonged periods of sitting, when rising from a seated position, and when climbing or descending stairs. X-rays and MRI are used to confirm that the arthritis affects only the patellofemoral compartment of the knee. Often, these images can be obtained on the same day as a visit to our Patellofemoral Center. For many patients with patellofemoral arthritis, non-operative treatment works well, and results in greater comfort and mobility. Patellofemoral joint replacement is recommended only if these measures are not successful and the patient’s quality of life is significantly affected.
At the Hospital for Special Surgery Patellofemoral Center, patients undergoing patellofemoral joint replacement receive regional anesthesia—an epidural block that numbs the lower half of the body—and sedation. During the operation, the orthopedic surgeon removes the damaged cartilage and a small amount of bone and places a high-density plastic patella (called a patellar button) in its place. Damaged cartilage and a small amount of bone are also removed from the groove on the femur and a thin metal laminate is put in its place, with the goal of restoring a gliding joint with minimal friction between the surfaces. The surgery takes about an hour to perform and requires an overnight stay in the hospital. [Watch video descriptions of patellofemoral surgery]
Recovery from Joint Reconstruction
Immediately after surgery, patients can put weight on the leg and are able to walk with the aid of a cane or crutches. Physical therapy usually begins a week after the patient returns home. Depending on the nature of the patient’s employment and his or her commute, time until return to work is between two and six weeks; full recovery from patellofemoral joint replacement—which is dependent primarily on the restoration of muscle strength—takes between six and twelve months. Measures that can help speed recovery include devices that provide electric stimulation to the muscles around the knee and Game Ready®, a machine that compresses and cools the leg, thereby reducing swelling and pain. (Insurance does not presently cover the cost of these devices.)
References
Summary by Nancy Novick


