Surgery for Neurofibromatosis Type 1

- What is neurofibromatosis?
- What are the symptoms of neurofibromatosis type 1?
- What are the orthopedic complications?
- How is it diagnosed?
- Scoliosis and kyphos in neurofibromatosis type 1
- Neurofibromatosis type 1 and bowing of the tibia
- What is the surgery for the orthopedic complications?
- Non-orthopedic surgeries / collaborative approach
What is neurofibromatosis?
Neurofibromatosis is a genetic disorder characterized by tumors known as neurofibromas, which grow in the nervous system and under the skin. This disease occurs as two distinct types: neurofibromatosis type 1 (NF1), which is more common, and neurofibromatosis type 2 (NF2).
NF1 affects about one in every 3000 people. NF2 affects only about one in every 25,000 people. NF2 does not frequently cause orthopedic problems. For this reason, this article focuses on issues related only to NF1.
What are the symptoms of neurofibromatosis type 1?
The two most common symptoms are neurofibromas (soft, pea-sized benign tumors on or under the skin, and multiple flat, light brown skin discolorations, sometimes referred to as “café-au-lait spots.” Freckles in the underarms or groin area may also be present.
Other symptoms can include:
- Face disfigurement – may occur when larger growths, called plexiform neurofibromas, affect the myriad nerves located on the face.
- Lisch nodules – tiny bumps on the iris of the eye (with no vision impairment).
- Optic pathway glioma – a tumor on the nerve connecting the eye to the brain.
- Bone deformities and orthopedic complications.
What are the orthopedic complications of neurofibromatosis type 1?
The two most common are spine deformities, particularly scoliosis − a lateral (sideways) curvature of the spine − and tibial dysplasia, in which the tibia (shin bone) bows and, thereby, fails to develop appropriately. Patients with tibial dysplasia are more susceptible to fractures and are at risk to develop tibial pseudarthrosis, in which the broken tibia heals with fibrous rather than bony tissue. Tibial dysplasia can also result in limb length discrepancy, where one leg is longer than the other. Other children with NF1 may develop a larger and longer leg without having any underlying bone problems. In these cases, the cause is overgrowth of soft tissues in the limb.
NF1 is associated with “acoustic neuromas” that may affect a person’s hearing and balance.
How is neurofibromatosis type 1 diagnosed?
A diagnosis of neurofibromatosis type 1 is made in children with two or more of the following criteria:
- skin lesions (neurofibromas)
- multiple spots on the skin that are darker than a patient’s normal skin tone (sometimes called “café au lait” spots because on people with lighter skin tones, they are similar in color to coffee with milk)
- freckling in the groin and underarms, eye abnormalities, including lisch nodules (tiny, pigmented tumors in the iris)
- particular skeletal abnormalities such as scoliosis or tibial dysplasia
- a family member with NF1


“Café au lait” spots (left) and axillary freckling of the underarm (right)
In cases where diagnostic findings are not conclusive, but neurofibromatosis is suspected, the child should be closely monitored by a multidisciplinary team that includes a pediatric neurologist and a geneticist.
Scoliosis and kyphosis in neurofibromatosis type 1
Children with NF1 who develop scoliosis may be diagnosed with either nondystrophic or dystrophic (degenerative) forms of scoliosis. Dystrophic scoliosis worsens quickly and unrelentingly.
Nondystrophic scoliosis symptoms and treatments
The condition resembles adolescent idiopathic scoliosis, with similar types of curves and curve patterns.
Treatment for nondystrophic scoliosis can include bracing as well as surgery. Instrumentation is used to realign the spine, and bone grafting is performed to help achieve spinal fusion. While the health risks associated with nondystrophic scoliosis are less pronounced, these curves can modulate into dystrophic scoliosis over time and, therefore, need to be monitored carefully until the child reaches skeletal maturity.


Posteroanterior (back-to-front) X-rays of dystrophic (first image) and nondystrophic scoliosis (second image)
Dystrophic scoliosis symptoms and treatments
In cases of dystrophic scoliosis, we typically see shorter, more sharply angulated curves. Characteristics of dystrophic scoliosis also include several bone abnormalities, including thinning of the ribs, significant rotation of the vertebrae, vertebral wedging, and erosion of the vertebrae by the spinal fluid, owing to the poor quality of the bone. Dystrophic scoliosis is also associated with kyphosis or a forward tilt of the spine, which can progress rapidly and may result in impingement of the spinal cord.
Due to the risks associated with NF1, orthopedic surgeons usually recommend surgery at a smaller curve magnitude (between 20 and 40 degrees) than with nondystrophic scoliosis. In contrast, surgery is recommended for idiopathic scoliosis patients with curves that exceed 50 degrees. Bracing is usually not an option in cases of dystrophic scoliosis.
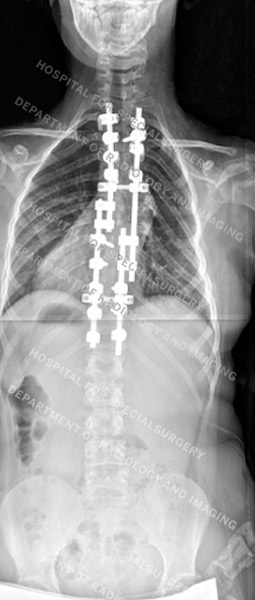

Posteroanterior (back-to-front) X-rays of dystrophic scoliosis (first image) and nondystrophic scoliosis (second image) after surgery
Neurofibromatosis type 1 and bowing of the tibia
Unlike the benign bowing of the legs that is not uncommon in healthy young children, the bowing of the tibia that is associated with neurofibromatosis has a distinctive orientation − an anterolateral bow (see figure below). This may lead to fracture and tibial pseudarthrosis (non-union). In such cases, surgical intervention is recommended. This is especially the case if the condition affects a child’s gait or ability to walk. Surgery can restore or improve walking function.

Anteroposterior (front-to-back) X-ray showing an anterolateral bowing in the tibia of a young patient
What is the surgery for neurofibromatosis type 1 orthopedic complications?
Although surgery is not always necessary, when appropriate, the primary surgeries involved in treating orthopedic complications of neurofibromatosis Type 1 include:
- Bone grafting with an intramedullary rod for pseudarthrosis, where an intramedullary rod is placed inside the bone to promote healing.
- Limb lengthening surgery for tibial dysplasia resulting in a limb length discrepancy.
- Spinal fusion for scoliosis and, if present, kyphosis. This surgery involves realigning the spine and using metal rods and screws with bone grafts to achieve fusion.
Surgery to correct a dystrophic scoliosis curve can present special challenges, including the need to correct a kyphotic (rounding of the back) curve at the same time. These surgeries also carry a risk of pseudoarthrosis or non-union. To help minimize this risk, orthopedic surgeons at HSS use autograft from the patient’s iliac crest bone (part of the pelvis) to achieve the fusion, as opposed to the allograft often used in other scoliosis surgeries. These complicating factors often necessitate more than one surgery.
Non-orthopedic surgeries and a collaborative clinical approach
Children with neurofibromatosis often require surgical and nonsurgical care across a variety of medical disciplines that may include orthopedics, neurology and neurosurgery, dermatology, oncology and others. HSS orthopedic surgeons and colleagues in other areas of medicine at Weill Cornell Medicine and Memorial Sloan Kettering Cancer Center are affiliated with and collaborate at the Neurofibromatosis Surgery Program at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. This cross-disciplinary approach provides an individualized treatment plan to optimize our patients’ outcomes.
Looking to the future
While there is no cure for neurofibromatosis, careful monitoring and intervention for orthopedic and other complications significantly improve the patient’s quality of life.
Learn more about the Pediatric Orthopedic Service.


