Transfemoral Osseointegration for a Patient with a Very Short Residual Femur After Amputation
From Grand Rounds from HSS: Management of Complex Cases | Volume 11, Issue 2
Case Report
A 25-year-old man presented 2 years after having undergone a left transfemoral amputation following a car accident. He reported extreme difficulty in fitting a socket prosthesis due to a short residual left femur. Multiple prosthesis fittings did not result in comfortable ambulation.
Physical examination revealed a left femur that measured 10 cm from groin to limb’s end, full strength, slight abduction and flexion contractures, and healthy skin that was not excessive (Fig. 1). His gait featured a short stance phase on his amputated side, with side-to-side sway and left-sided pelvic elevation to maneuver the prosthesis. Radiographs identified 6.5 cm residual femur beyond the lesser trochanter with slight distal heterotopic ossification and no hip joint arthrosis (Fig. 2). A long standing radiograph identified features typical of transfemoral amputation: a net femur abduction of 21° (femur anatomic axis 14° abduction vs the right’s normal 7° adduction), a medial mechanical axis deviation of 28 mm, and a prosthesis that was too short by 12 mm (imparting a 5° pelvic obliquity) to facilitate swing-through (accommodating the prosthetic limb’s sag during gait).
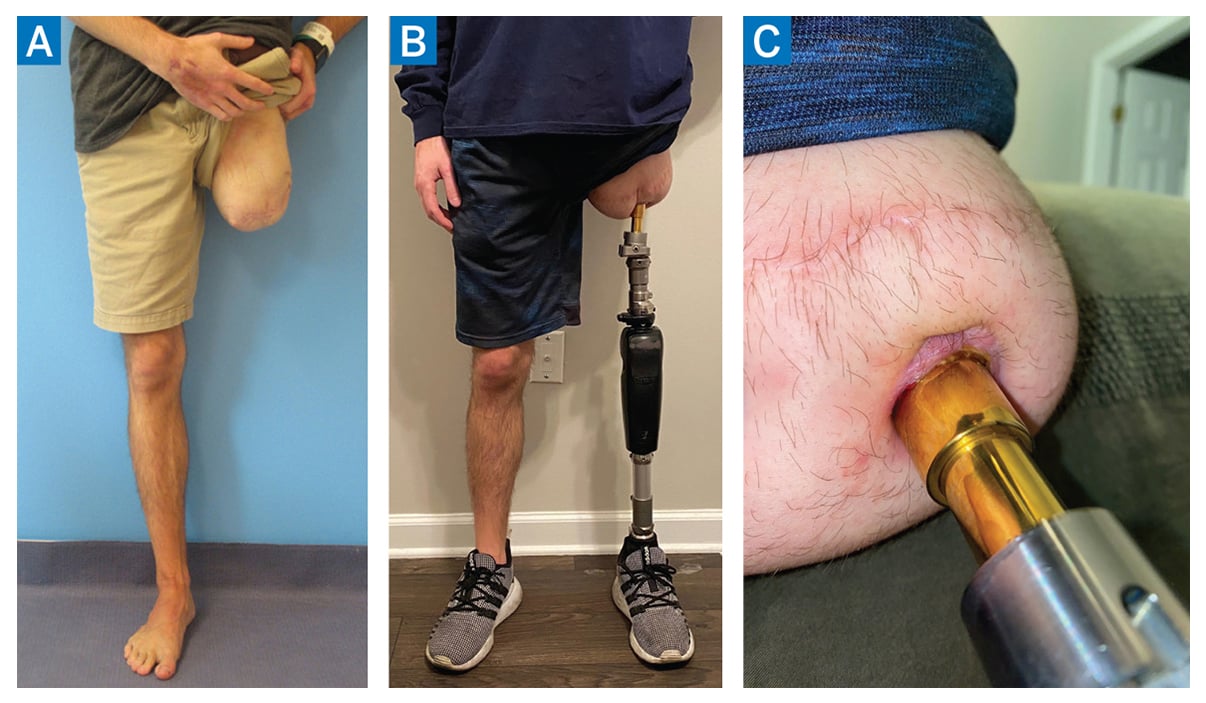
Figure 1: Clinical photographs of the patient. (A) Preoperative photo identifying left transfemoral amputation with slight abduction and flexion contractures of the hip joint, and healthy skin without excess bulk. Postoperative photos 1.5 years after osseointegration identifying (B) balanced stance and (C) healthy stoma surrounding the transcutaneous implant.
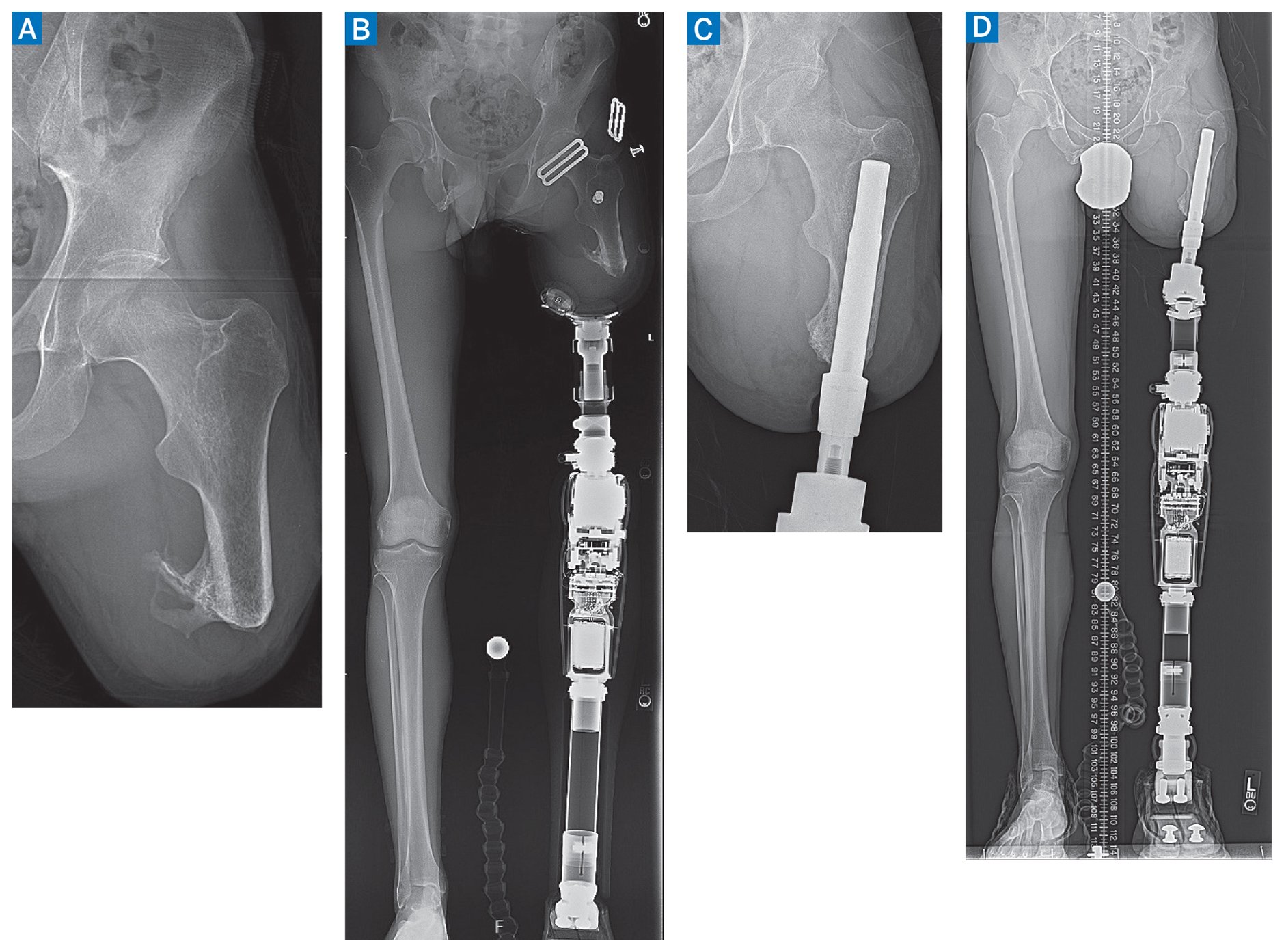
Figure 2: Preoperative radiographs (A, B) identify the amputated femur with joint abduction contracture and mechanical axis deviation. His postoperative radiographs (C, D) identify a stable osseointegrated prosthesis, neutral mechanical axis, and level pelvis.
The patient underwent a transcutaneous osseointegration to implant a skeletally anchored prosthetic limb adapter, along with revision amputation of the heterotopic bone and a plastic surgery-assisted thigh lift to remove excess soft tissue. To prepare for this, preoperative computed tomography (CT) was performed to fabricate a custom titanium implant (Fig. 3).
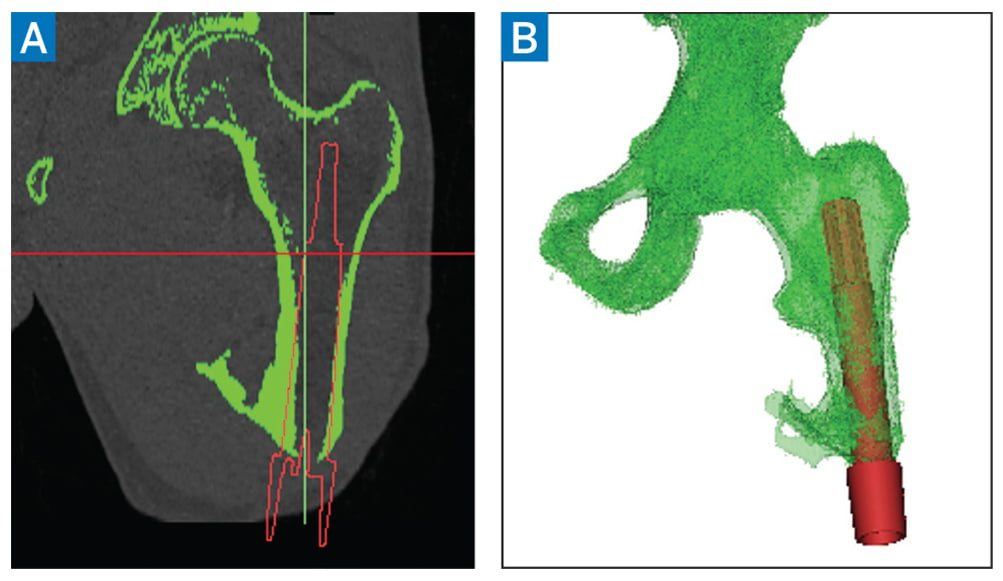
Figure 3: Preoperative computed tomography scan. Initial renderings (A) allow volumetric reconstruction to model the patient-specific implant (B).
The patient has made excellent progress through 18 months of follow-up. His gait is nearly completely natural. The stoma surrounding the transcutaneous implant is healthy (Fig. 1). Radiographs (Fig. 2) identify the osseointegrated prosthesis is stable with the long standing radiograph showing his femur has identical alignment to his unaffected side. His leg lengths have minimal difference which achieves a level pelvis, and his mechanical axis is directly through the knee joint. His mobility and enjoyment of life have markedly improved.
Discussion
Transcutaneous osseointegration is a novel reconstructive option for rehabilitation in patients who have had an amputation [1]. The first clinically successful procedure was performed in 1990; pressfit techniques began in 1999 but have been performed in greater numbers only in the past decade [2]. HSS is the only US center to routinely perform press-fit osseointegration, with our service performing our first procedure in 2017. We’ve had fantastic success in improving patients’ mobility, quality of life, and satisfaction [3]. For some patients, we have partnered with plastic surgeons to provide targeted muscle reinnervation, which helps relieve neuroma and other nerve-related pain [4]. While most patients who undergo osseointegration after amputation have had a traumatic etiology, it is also safe and effective in treating patients with oncologic amputation [5], can accommodate myoelectric and computerized prosthetic limbs [6], and is advantageous from a cost perspective [7].
Based on our positive experience, we have created an Osseointegration Center that will help us lead the upcoming Food and Drug Administration validation trial.
View Videos on Osseointegration Techniques:
References
- Reif TJ, Jacobs D, Fragomen AT, Rozbruch SR. Osseointegration amputation reconstruction. Curr Phys Med Rehabil Rep. 2022. doi: 10.1007/s40141-022-00344-9.
- Hoellwarth JS, Tetsworth K, Rozbruch SR, Handal MB, Coughlan A, Al Muderis M. Osseointegration for amputees: current implants, techniques, and future directions. JBJS Rev. 2020;8(3):e0043. doi: 10.2106/JBJS.RVW.19.00043.
- Reif TJ, Khabyeh-Hasbani N, Jaime KM, Sheridan GA, Otterburn DM, Rozbruch SR. Early experience with femoral and tibial bone-anchored osseointegration prostheses. JBJS Open Access. 2021;6(3):e21.00072. doi: 10.2106/JBJS.OA.21.00072.
- Marano AA, Modiri O, Rozbruch SR, Otterburn DM. Soft tissue contouring at the time of osseointegrated implant reconstruction for lower extremity amputation. Ann Plast Surg. 2020;85(S1 Suppl 1):S33-S36. doi: 10.1097/SAP.0000000000002329.
- Reif TJ, Fragomen AT, Rozbruch SR. Percutaneous osseointegration prosthesis. In: Özger H, Sim FH, Puri A, Eralp L, editors. Orthopedic Surgical Oncology for Bone Tumors: A Case Study Atlas. Cham: Springer; 2022, p. 265–72. doi: 10.1007/978-3-030-73327-8_26.


