Lupus Nephritis: What You Should Know About Lupus and Kidney Disease

Joint pain and swelling, skin rash, fatigue and fever are often the primary symptoms of systemic lupus erythematosus (SLE), or lupus, but people with this autoimmune condition face a variety of health challenges that affect other organs, including the heart and lungs. Between 30% to 50% of those diagnosed with lupus will develop kidney disease, also known as lupus nephritis, within the first six months to three years of their condition.
What causes lupus nephritis?
In people with lupus, the immune system mistakenly regards its own tissues as foreign substances, setting off a response that leads to tissue inflammation. In otherwise healthy people, inflammation is a normal and temporary part of the immune response. However, in a person with SLE or other types of autoimmune disease, inflammation can become chronic, resulting in damage to joints or organs.
Although autoimmune diseases like lupus can affect all parts of the body, the kidneys may be particularly vulnerable to damage as structures called immune complexes (a combination of an antibody and the ostensibly “foreign material” it is combating) develop and deposit in the kidneys. Once there, they cause both inflammation and alterations in the anatomy of the kidney that result in the loss of protein and/or blood cells in the urine. Of note, each kidney is composed of about 1 million functional units, called nephrons. Each nephron is made of a glomerulus (glomeruli in plural) where the blood is filtered and waste products are excreted as urine. The vessels in the glomerulus that filter waste out of the blood are porous and permit the immune complexes to enter the kidney tissues and cause kidney inflammation (nephritis).
What are the signs and symptoms of lupus nephritis?
Signs of lupus nephritis may include:
- swelling or puffiness of feet, legs, eyes
- high blood pressure
- high protein levels in the urine
- frothy urine or getting up constantly to urinate at night
- blood in the urine
You may not experience any symptoms, however, so a urine test is needed. It is crucial to have your doctor rule out other causes such as kidney stones or a urinary tract infection before considering the diagnosis of nephritis.
Who is most at risk for lupus nephritis?
For reasons that are not yet fully understood, women develop lupus far more frequently than do men (at a ratio of 9:1) and women of African, Asian and Hispanic descent are at greater risk than their Caucasian counterparts, which suggests a genetic cause. The disease usually occurs during the reproductive years. Similarly, lupus nephritis is seen more frequently in women.
Moreover, lupus nephritis usually develops in people with more severe forms of lupus.
How do you diagnose and test for lupus nephritis?
In addition to conducting a thorough physical examination and patient history, doctors use a wide range of tests to assess kidney function. These include measuring creatinine – a waste product related to normal tissue breakdown, as well as levels of certain antibodies and other proteins in the blood and urine. The presence of high levels of anti-DNA antibodies, and lower than normal levels of proteins called Complement 3 and Complement 4 not only help to confirm a diagnosis of lupus but also appear to indicate an increased risk of developing lupus nephritis.
Below is a comprehensive list of additional tests that rheumatologists and other physicians may review when assessing how lupus nephritis and its treatment may be affecting other systems and organs:
- Blood: BUN (normally<20) and creatinine (Cr; normally <1 in the average woman; it may be higher in muscular men as it reflects muscle mass). Also albumin (normal>3.5) which may be decreased due to loss of protein in the urine.
- Electrolytes: sodium, potassium, bicarbonate
- Creatinine clearance: Calculated by using creatinine, age, race, gender. Normally 80-120 ml/min/1.73m2
- Urine analysis: Normally 0-trace protein, no red and white blood cells (<5 RBC, <5 WBC)
- 24-h urine protein: (creatinine is also measured to assess whether collection was performed properly): normally <300mg/24h. In lupus nephritis >500 mg/24h.
- Spot urine protein/creatinine ratio: Normally <0.3 (in grams of protein per gram of creatinine). It may vary depending on the timing of collection: best to test second urine of the day
- Kidney biopsy (see below)
Other Important Tests:
- Serology:
- C3 (normally>80). When disease is active, it is usually low
- C4 (normally>18). When disease is active, it is usually low
- Anti-dsDNA. When disease is active, it is usually present
- Antiphospholipid antibodies (anticardiolipin antibodies IgG, IgM, IgA; beta2 glycoprotein I antibodies IgG, IgM, IgA; and lupus anticoagulant). This might determine whether blood thinners are needed
- Bone tests:
- Blood level of 25-OH-Vitamin D (normal >30 ng/ml)
- Blood level of intact parathyroid hormone (iPTH; it is usually high in advanced kidney disease or with low 25-OH-Vitamin D levels)
- Bone mineral density test (to check for osteoporosis)
- Fasting lipids: High in nephrotic syndrome
- Fasting blood sugar: Diabetes or other complications of steroids
- Hemoglobin (HB): Low HB (anemia) might be due to the inflammation, blood loss, hemolysis, or advanced kidney disease.
- White blood cells: Low due to lupus or therapy. Increased risk of infection.
- Platelets (PLT): Low due to the lupus or therapy. Increased risk of bleeding.
- Purified protein derivative (PPD) test for latent tuberculosis (TB)
- Hepatitis C, Hepatitis B, HIV
Additional tests, such as a renal (kidney) ultrasound, may be needed to exclude other kidney problems that may need a different treatment than lupus nephritis. Before beginning treatment, it is very important to determine that the patient’s kidney problems are being caused by lupus nephritis and not by another condition such as an infection or an obstruction like a kidney stone.
If the physician suspects that lupus nephritis is causing the symptoms and abnormal laboratory results, he or she will often also recommend a biopsy. In this procedure, which is usually performed by a nephrologist using a special needle under ultrasound or other radiographic guidance, a small piece of tissue is removed from the kidney. Biopsies reveal whether any changes have occurred in the cells of the kidney and whether there is any scarring present. [Figures 1A and 1B] Information gathered with a biopsy is an important tool in determining the course of treatment.
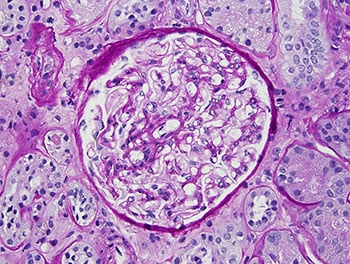
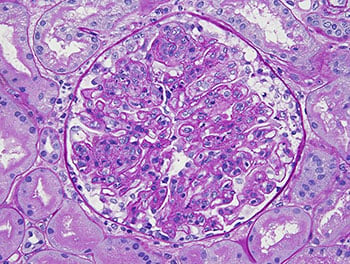
Figure 1A (left): Kidney biopsy showing a normal glomerulus.
Figure 1B (right): Kidney biopsy from a patient with class IV lupus nephritis showing a glomerulus
with narrowing/closing of the capillaries (small blood vessel) from an abnormal increase of cells within those vessels.
Lupus nephritis classification
Lupus nephritis is diagnosed according to the 2003 International Society of Nephrology/Renal Pathology Society (ISN/RPS) classification of lupus nephritis:
- Class I, also called minimal mesangial lupus nephritis
- Class II, also called mesangial proliferative lupus nephritis
Both Class I and Class II are mild forms of the disease that do not require treatment.
- Class III, focal lupus nephritis
- Class IV, diffuse segmental (IV-S) or global (IV-G) lupus nephritis
Class III and Class IV are serious forms of the disease, with the two types of Class IV being more aggressive than class III.
- Class V disease, or membranous lupus nephritis may occur by itself or in combination with class III or class IV.
When Class V occurs by itself, it can take two forms depending on whether the individual has nephrotic proteinuria (the presence of high levels of protein in the urine) or non-nephrotic proteinuria.
- Nephrotic proteinuria is defined as protein loss of 3.5 grams or greater over a 24-hour period; this condition may be associated with a higher risk of developing blood clots.
- Class V nephritis with non-nephrotic proteinuria is a less severe condition in which the loss of protein through the urine is less than 3.5 grams over a 24-hour period.
In the case of classes III and IV, the biopsy will also indicate the proportion of glomeruli with inflammation (active) and with scar tissue (sclerotic). The presence of more aggressive forms of inflammation such as “crescents” and “fibrinoid necrosis” will also be indicated.
In all classes, the biopsy comments on the presence, type, and degree of tubular, interstitial (the tissue between kidney units) and vascular involvement.
If a person is found to have Class VI disease, or advanced sclerosing lupus nephritis, the kidney contains only scar tissue without active inflammation, and therefore aggressive treatment with immunosuppressive drugs is not indicated. Patients with this type of lupus nephritis will not benefit from medication and are started on dialysis.
How do you treat lupus nephritis?
People with the more severe forms of lupus nephritis, classes III, IV and V (with nephrotic proteinuria), need to be started on an aggressive course of treatment that is also referred to as induction therapy, since the goal is to induce a remission of the inflammation and related symptoms. During induction therapy, immunosuppressive drugs are administered at high doses. The duration of induction therapy can range from three months to one year. A key point here is to start induction therapy as soon as possible without losing time, in order to minimize loss of kidney tissue from the inflammation. “Time is kidney,” as many doctors say.
As the condition improves, the patient switches to maintenance therapy, in which a lower dose of the drug or drugs is administered. Maintenance therapy continues for at least two years, though the optimal duration is not known yet.
Because immunosuppressive agents are powerful drugs with the potential for serious side effects, the rheumatologist strives to taper their use as soon as the condition allows.
Immunosuppressive agents include:
- High dose glucocorticoids (or steroids) such as prednisone (by mouth) or methylprednisolone administered by mouth, often after IV infusions of methylprednisolone for ne to three days.
- Intravenous administration of cyclophosphamide every month for a period of six months.
- Oral mycophenolate.
- Oral azathioprine. This medication is not the first choice for induction or maintenance therapy. However, it is used in certain situations such as pregnancy or intolerance to the other drugs.
- Other agents that may occasionally be used include: cyclosporine, tacrolimus, rituximab, etc.
Adjunctive therapy that addresses other disease-related concerns may include one or more of the following, depending on the individual case and if there are no contraindications:
- Diuretics, to reduce swelling and control blood pressure
- Angiotensin Converting Enzyme (ACE) inhibitors and Angiotensin Receptor Blockers (ARBs), additional drugs that help control high blood pressure and reduce proteinuria
- Bisphosphonates, such as alendronate, to protect the bones
- Statins and other drugs that control cholesterol
- Anticoagulants for people at risk of blood clots
- Antibiotics such as Trimethoprim/Sulfamethoxazole protect against PJP pneumonia (during periods of heavy immunosuppression) and vaccines protect against other infections such as pneumococcal pneumonia or the flu.
Initially, some people with very severe lupus nephritis may need to be hospitalized while receiving treatment. This is done to ensure that any complications of the disease or treatment can be addressed promptly. However, many people with lupus nephritis are able to receive specific treatment including therapeutic infusions on an out-patient basis.
Treatment guidelines and warnings
Treatment for lupus nephritis can be complicated. Both lupus itself and the drugs taken to manage the disease can put the patient at greater risk of infection, cardiovascular disease, risk of stroke, osteoporosis, and weight gain. Glucocorticoid (steroid) therapy alone is associated with many adverse effects such as weight gain, osteoporosis, and osteonecrosis (bone damage that may lead to severe arthritis of the hip and need for surgery).
The goal is to control the disease as quickly as possible, and then reduce the dose of medications given, to limit side effects. Fortunately, younger patients usually tolerate immunosuppressive drugs better, and lupus primarily affects this younger population. Many patients show rapid improvement with induction therapy.
Unfortunately, people who are successfully treated for lupus nephritis remain at risk of recurrence for the condition. Therefore, regular monitoring of kidney function is essential, especially since the early signs of recurrence may only be detectable with laboratory tests.
People undergoing treatment for lupus nephritis are also advised to follow various guidelines regarding diet, nutritional supplements, and over-the-counter drugs.
- All patients will need to limit the amount of salt in their diet, because it can cause fluid overload and leg swelling.
- If they are taking prednisone, which can increase the risk of osteoporosis, it is important to supplement the diet with calcium and vitamin D.
- People with lupus nephritis should eat a healthy diet, maintain a healthy weight and avoid taking non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, which place further stress on the kidneys.
- They should also avoid the IV contrasts that are administered with some CT scans and MRIs, unless they are absolutely necessary.
In addition to physical challenges, a diagnosis of lupus nephritis can also take a psychological toll. For those having difficulty coping, family support and social work services may help.
If lupus nephritis is active, pregnancy is not just inadvisable, but can be life-threatening. However, in cases where treatment results in a period of quiescence or inactivity for six months, without much kidney damage, and with careful adjustment of medications, a safe pregnancy is the rule. Patients who undergo successful transplants may also be able to proceed with a safe pregnancy.
How should I take care of myself if I have lupus nephritis?
- Be active in your health care and partner with your rheumatologist and nephrologist (doctor who specialize in kidney diseases).
- Be aware of what pills you are taking, their dosage, and when to take them.
- Recognize the different signs of flares relating to the disease, such as headache, high blood pressure, discolored urine, fever, joint pains, skin rash, shortness of breath, and foot/eye swelling. Notify your doctors.
- Recognize the signs of potential drug adverse events such as fever, chills, sore throat, cough, shortness of breath, blood in urine and diarrhea. Notify your doctors.
- Take care of your bone health (ensure adequate intake of calcium/vitamin D through food or supplements) and your cardiovascular health (quit smoking, eat a low saturated fat diet).
Where can I get treatment for lupus nephritis?
Timely and aggressive treatment results in considerable improvement or complete remission in many people, but treatment is not yet optimal for all patients. Those who do not respond to conventional treatment may be eligible for clinical studies of newer agents. At the HSS Lupus and APS Center of Excellence, people with lupus nephritis benefit from multidisciplinary care from a team of rheumatologists, nephrologists, pathologists and other specialists, an on-site infusion service, social work and other support services, all in one location.
Many of the Center’s faculty members are engaged in clinical research designed to improve treatment outcomes. Researchers and physicians at HSS and across the country continue to evaluate the possible role of other medications to effectively treat lupus nephritis and minimize the risk of side effects.
Please visit our Lupus Nephritis Program page for more information.
If you would like more information about the treatment of lupus nephritis at HSS, please request an appointment or call 1.877.606.1555.
Acknowledgement
We thank our trusted colleague, Dr. Surya V. Seshan, Professor of Clinical Pathology and Laboratory Medicine at Weill Cornell Medicine, for her kind provision of the kidney biopsy pictures used in this article and for her helpful comments.

