Hand Problems: Common Injuries, Arthritis and Trigger Finger
Hand problems vary in severity, but even minor injuries can have a major impact on your daily life. A hand surgeon can help determine the cause of your symptoms and customize a plan of care to get your hands feeling and working well again. Learn about some common hand problems and how they are treated.

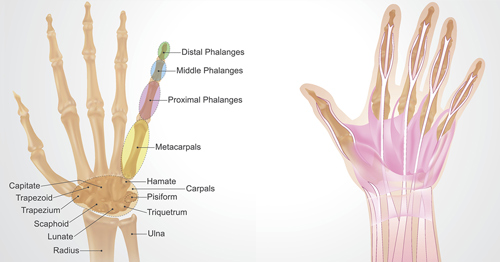
Anatomy of the hand
Your hand contains 19 bones (not including those that form the wrist). There are 14 phalanges, the bones that make up each finger: three in each of the index, middle, ring, and pinky fingers and two in the thumb. There are also five metacarpal bones that make up the middle part of the hand. Numerous ligaments connect the bones to each other. Tendons connect muscles in the arm or hand to the bone to enable you to move your fingers. Sheaths are tubular structures that surround part of the fingers. There are thousands of nerve endings in your fingertips. Arteries, veins, and nerves provide essential blood flow and sensation in the hand and fingers.
Common injuries hand surgeons treat
The hand is one of the most complex structures in the body, and trauma can injure not only the skin or bones of the hand, but also delicate nerves, arteries, tendons, and ligaments that allow your hand to function properly. When surgery is required, this complex network can be challenging to navigate, requiring the expertise of an experienced hand specialist. Hand surgeons are orthopedic surgeons with additional, advanced training in methods for treating upper extremity conditions. This includes performing surgery under a microscope, which may be necessary for fixing small structures in the hand and fingers.
The hand is commonly injured during sports, work or daily life activities. Common types of injuries that hand surgeons often treat include:
- cuts from knives or sharp glass
- falls on the outstretched hand
- crush injuries of the hands or fingers, such as catching them in a door
- sports-related acute and overuse injuries
- animal bites and scratches
- injuries from power tools, such as circular saws or drills
Seeing a hand specialist soon after an injury can assure that you get the most effective treatment as soon as possible. The surgeon will ask you how the injury happened and perform a physical exam to examine the skin for any swelling or bruising and to assess your range of motion. Imaging tests such as X-rays, MRIs, and CT scans can provide additional information. Hand surgeons at some institutions have access to advanced imaging techniques like 3D CT reconstruction and 3D printing of your bones. Your surgeon will speak with you about your usual activities and hobbies so he or she can devise a plan of care to get you back to those activities.
Many hand injuries can be treated with splints, casts, and hand therapy. Hand surgeons work closely with hand and occupational therapists to create a personalized therapy approach that is right for each patient. In some cases, hand surgery is needed to fix broken bones or repair injured nerves, ligaments, or tendons. Most hand surgeries can be done in the outpatient setting, using a nerve block for pain control. Your surgeon and team will work together to ensure a safe surgery and a smooth recovery.
Full recovery from a hand injury depends on the severity of the injury: six weeks for most fractures, but up to several months or a year for certain nerve injuries. Your hand surgeon and hand therapist will work closely with you after surgery to help you recover as quickly as possible so you can get back to doing the things you enjoy.
Hand arthritis: Symptoms, signs and treatments
Arthritis is inflammation of cartilage in the joints, which causes swelling and pain. There are two basic types of arthritis that most commonly affect the hand and fingers: osteoarthritis and rheumatoid arthritis.
- Osteoarthritis is the most common type of arthritis and usually affects the hands of older people resulting from years of use. Similar to that of arthritis in larger joints, such as the hip and knee, there are multiple treatment options for hand osteoarthritis to help patients get back to the activities they love.
- Rheumatoid arthritis (RA) can also cause similar pain and swelling in the joints, but this condition is caused by an autoimmune disorder, rather than wear over time, and so it can reduce hand function earlier in life than is common for osteoarthritis. Fortunately, with the advent of biologic therapies, people with RA are experiencing fewer serious hand problems and the disease's progression has been dramatically slowed.
If you show signs of hand arthritis, your doctor will begin with a physical examination, look for points of tenderness, and assess the degree of stiffness. Imaging studies such as X-rays and MRI can be used to determine the extent of the degenerative changes.
Nonsurgical treatments for hand arthritis
Depending on which joints are affected – the first knuckle below each fingernail is the most common hand joint impacted by arthritis – your treatment may include a combination of anti-inflammatory medications (such as ibuprofen or naproxen), rest, ice, wearing a splint, and/or receiving a cortisone injection to relieve inflammation. A hand therapist may be helpful to teach you new ways to use your hands to do what you want to do despite your arthritis.
Surgery for hand arthritis
Surgery is a last resort, but in patients with arthritis causing severe pain, it can be very successful. For arthritis affecting the base of the thumb (called basal joint arthritis), the most common surgical procedure is removal of a bone called the trapezium and reconstruction of the joint with tendons and/or sutures. After surgery, your hand will be placed in a splint or cast while it heals, and then you will receive regular hand therapy to help regain strength and function.
Trigger finger: Symptoms, signs and treatments
Also called "stenosing tenosynovitis," trigger finger makes it difficult to fully straighten or bend your fingers. You may be unable to make a fist. People with trigger finger often feel their symptoms are worse when they wake up in the morning. While trigger finger can affect any finger, it most commonly arises in the ring finger, middle finger, and thumb.
Flexor tendons attach the muscles of your forearm to the bones of your fingers, passing through tunnels in the palm. When you contract a muscle in your arm, the flexor tendons enable your fingers to bend. With trigger finger, bands of tissue called "pulleys" that hold the flexor tendons close to the finger bones become inflamed or thickened, making it harder for the tendon to slide through the pulley as you bend your finger.
You may feel a small nodule in your palm that develops from enlargement of the tendon and/or thickening of the pulley. This may cause the tendon to catch as it passes through the pulley. You may also feel a clicking of the finger or experience locking of the joints. This is often quite painful and if left untreated, may lead to permanent stiffness of the finger.
Nonsurgical treatments
You'll have the best chance of a good recovery from trigger finger if you start treatment soon after your symptoms first appear. Your doctor may give you a cortisone shot into the affected area to relieve the inflammation. Massaging the area may reduce tendon swelling. Some people also benefit from wearing a splint at night to keep the affected finger straight.
Surgery for trigger finger
If conservative treatment measures aren't enough to make your symptoms go away, you may need surgery. The hand surgeon will cut the pulley to help the tendon glide smoothly, without catching or locking. You won't need a splint or cast but you'll need to protect the incision site from water to prevent infection. After four to eight weeks, you may experience some internal tissue firmness and skin sensitivity, but this generally resolves by 12 weeks after the operation. No hand therapy is required unless you need some additional exercises to stretch the fingers after you have healed.


