Neurolysis and Nerve Transfer for Iatrogenic Axillary Nerve Injury After Humeral Avulsion of the Glenohumeral Ligament Repair
From Grand Rounds from HSS: Management of Complex Cases | Volume 9, Issue 1
Case Report
A 39-year-old left-handed man presented with 2 years of numbness and weakness in the left shoulder following arthroscopic repair of a humeral avulsion of the glenohumeral ligament (HAGL) in his home country. He had previously undergone electrodiagnostic testing (EDX) and a magnetic resonance imaging (MRI) scan of the brachial plexus, which showed moderate-to-severe denervation of all 3 heads of the deltoid muscle and normal appearance of the brachial plexus.
Physical examination revealed marked deltoid atrophy and sensory deficits within the autonomous zone of the axillary nerve. Strength testing demonstrated an isolated British Medical Research Council (BMRC) [4] M4 strength deficit in left shoulder abduction. Active range of motion was full and symmetric. EDX demonstrated low discrete motor unit recruitment (1 to 2 motor units) in the anterior and middle heads of the deltoid, decreased recruitment (substantial but not full motor unit recruitment) and nascent motor unit action potentials (MUAPs) (evidence of axonal regeneration) in the posterior deltoid, and full motor unit recruitment in the teres minor.
Brachial plexus MRI showed the axillary nerve following an aberrant course between the intermuscular fat planes of the subscapularis and coracobrachialis, extending in a cephalocaudal direction toward the anteroinferior aspect of the glenohumeral joint (Fig. 1). The nerve appeared in continuity but tethered to the inferior glenohumeral ligament (IGHL) by a suture (Fig. 2). Diagnostic ultrasound further showed the axillary nerve extending superiorly toward the glenohumeral joint. Because the nerve remained in continuity and EDX demonstrated partial axillary nerve function, the patient was indicated for exploration and release of the axillary nerve.
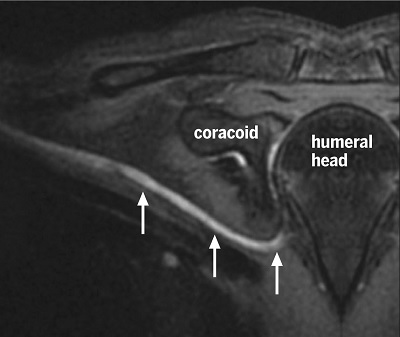
Figure 1: Curved, multiplanar reformatted T2-weighted inversion recovery brachial plexus MRI shows the axillary nerve (white arrows) following an aberrant course cephalocaudally toward the anteroinferior aspect of the glenohumeral joint.
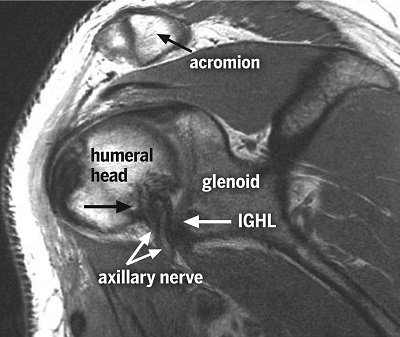
Figure 2: Oblique sagittal proton density-weighted MRI shows the axillary nerve tethered by suture (lower black arrow) to the inferior glenohumeral ligament (IGHL).
In the operating room, the patient was placed in the modified beach chair position to allow for anterior access. A multiwindow deltopectoral approach [5] was used to provide adequate anterior and posterior exposure of the axillary nerve. The deltopectoral groove was opened, and the axillary nerve, identified on the subscapularis, was traced to its division into anterior and posterior branches (Fig. 3). The nerve was found tethered at the 6 o’clock “blind zone” [3] position by capsular sutures that were raised and divided, freeing the nerve (Fig. 4). Electrical stimulation of the posterior branch demonstrated contraction of the posterior deltoid and teres minor; however, the anterior branch was severely constricted, and stimulation yielded no response. The wound was irrigated and closed to allow for repositioning of the patient in the lateral decubitus position. A posterior approach was subsequently employed to microsurgically transfer the long head of the triceps branch of the radial nerve to the anterior division of the axillary nerve (Fig. 5 and Fig. 6).
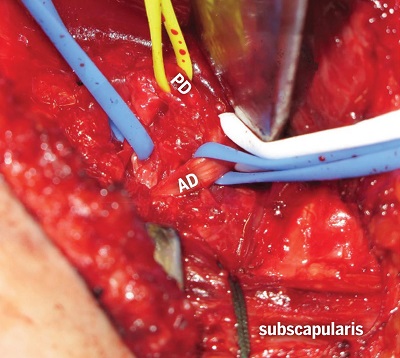
Figure 3: The subscapularis tendon is retracted with green suture, allowing the anterior division (AD) of the axillary nerve to be traced proximally to its tether point. The posterior division (PD) is retracted with a yellow vessel loop.
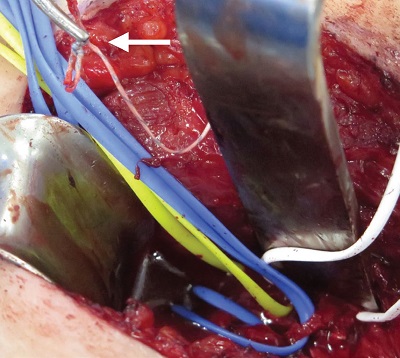
Figure 4: The anterior division of the axillary nerve is freed from tethering, with capsular sutures cut and removed (white arrow).
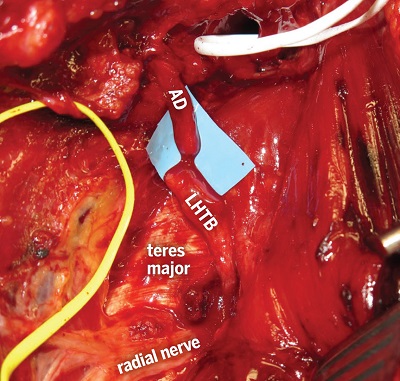
Figure 5: Long head of triceps branch (LHTB) reflected and prepared for nerve transfer to the AD of the axillary nerve, with a slit in the teres major extending the swing distance of the nerve. The PD of the axillary nerve is held by the white vessel loop.
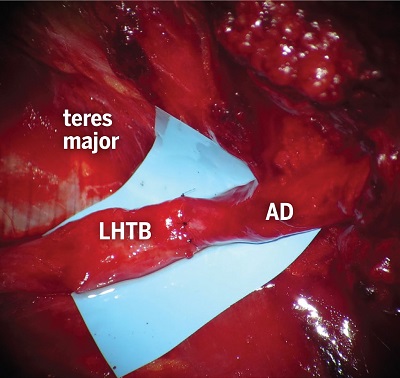
Figure 6: Microneurorrhaphy of the LHTB to the AD of the axillary nerve, demonstrating a good size match without tension.
Nine months following neurolysis and nerve transfer, the patient had M5 strength and full range of motion in his left shoulder, with residual diminished sensation over the autonomous region of the axillary nerve. EDX showed nascent MUAPs (axonal regeneration) in all 3 deltoid heads, decreased recruitment pattern in the middle and posterior heads, and discrete (limited) recruitment in the anterior head.
Discussion
This case highlights several important points about iatrogenic nerve injury following HAGL repair. First, although outcomes of arthroscopic and open HAGL repair are comparable [1], the risk and degree of impairment from axillary nerve injury may outweigh the perceived benefits of an arthroscopic approach [2].
Additionally, it is important for surgeons to know how to identify and manage patients with postoperative nerve injuries. A combination of diagnostic tools, including meticulous physical examination, EDX, and advanced, nerve-sensitive, high-resolution MRI scanning, can aid in the prompt identification and localization of iatrogenic nerve injury. In particular, MRI should be focused on the specific nerves in question to ensure the highest diagnostic yield. As this patient’s initial MRI showed, a conventional brachial plexus MRI may include a field of view encompassing only the takeoff of the terminal branches from the cord level and may not extend laterally enough to visualize the course of the axillary nerve as it traverses inferior to the glenohumeral joint and enters the quadrilateral space.
Lastly, the use of different surgical windows for exposure and treatment of axillary nerve injuries [5] may help overcome the difficulty of accessing the “blind zone” [3]. This area of the axillary nerve cannot be reached using standard shoulder or plexus approaches and may be the site at which a suture anchor can tether the axillary nerve during HAGL repair.
Posted: 3/2/2020
Authors
Drake G. LeBrun, MD, MPH
Orthopaedic Surgery Resident
Director, MR Neurography and Director, MRI Research, Hospital for Special Surgery
Attending Radiologist, Hospital for Special Surgery
Medical Director, Center for Brachial Plexus and Traumatic Nerve Injury
Attending Physiatrist, Hospital for Special Surgery
Chief, Division of Ultrasound, Hospital for Special Surgery
Attending Radiologist, Hospital for Special Surgery
Chief, Hand and Upper Extremity Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Attending Orthopedic Surgeon and Senior Scientist, Hospital for Special Surgery
Professor of Orthopedic Surgery, Wrist Surgery and Nerve Repair, Weill Cornell Medical College
References
- Bozzo A, Oitment C, Thornley P, et al. Humeral avulsion of the glenohumeral ligament: indications for surgical treatment and outcomes—a systematic review. Orthop J Sports Med. 2017;5:1–7.
- Carofino BC, Brogan DM, Kircher MF, et al. Iatrogenic nerve injuries during shoulder surgery. J Bone Joint Surg Am. 2013;95(18):1667–1674.
- Maldonado A, Howe B, Lawton R, Bishop A, Shin A, Spinner R. Anatomical study of the axillary nerve: description of a surgical blind zone. Plast Reconstr Surg. 2016;138:419–426.
- Medical Research Council. Aids to the investigation of the peripheral nervous system. London: Her Majesty’s Stationary Office; 1943.
- Perez A, Mahmood B, Jethanandani R, Lee S, Wolfe S. Overcoming the axillary nerve “blind spot” through the deltopectoral and axillary approaches: a cadaveric study. J Hand Surg Am. 2019 [in press]. https://doi.org/10.1016/j.jhsa.2019.11.013






