Plantar Fasciitis
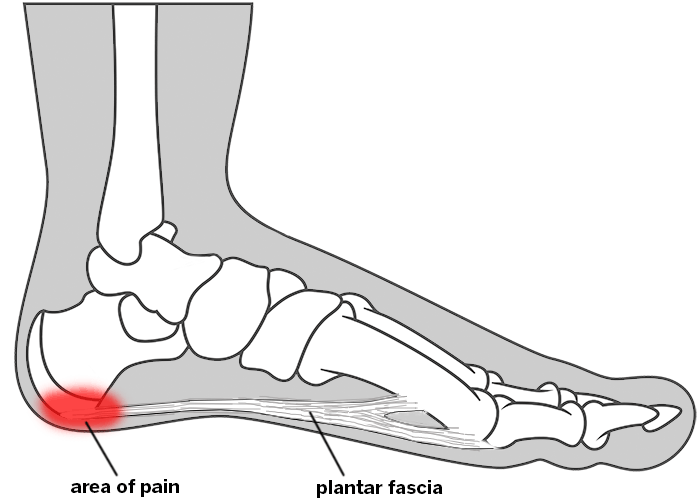
The plantar fascia is a thick, fibrous connective tissue that runs across the bottom of the foot, connecting the heel bone (calcaneus) to the ball of your foot. This tissue acts as a shock absorber and supports the arch.
- What is plantar fasciitis?
- What causes plantar fasciitis?
- How do I know if I have plantar fasciitis?
- How do you treat plantar fasciitis?
- Is there surgery for plantar fasciitis?
- What is the recovery time for plantar fasciitis surgery?
What is plantar fasciitis?
This is when the plantar fascia on the bottom of the foot becomes inflamed, leading to stabbing pain and tenderness in the heel area. The pain can make it difficult to bear weight and walk.
What causes plantar fasciitis?
Plantar fasciitis is normally a chronic condition that can be triggered by wearing unsupportive footwear, running or, sometimes, no clear reason. Contributing factors include age, individual foot anatomy, being overweight, and jobs or leisure activities that put repetitive stress on a person's foot.
Risk factors
- Age: Plantar fasciitis most commonly begins around the age of 40.
- Foot anatomy: People with flatfeet, high arches or alignment issues such as over pronation.
- Being overweight or obese: Extra weight adds stress to the feet.
- Occupation: Jobs that require long hours of standing or walking can stress feet over time, especially if you have other risk factors listed here.
- Exercise that puts stress on the heel that involves running, jumping and dancing.
How do I know if I have plantar fasciitis?
The main symptom of plantar fasciitis is intense pain in the heel area that is often worse in the morning and improves throughout the day. The pain is generally concentrated where the ligament meets the base of the heel.
An ultrasound, X-ray or MRI may be necessary to diagnosis the condition and rule out other possibilities, such as a stress fracture or a heel spur.
Plantar fasciitis is sometimes confused with a heel spur, which is a bone spur on the bottom of the calcaneus (heelbone). Although the two conditions can both be present and connected, they can also occur independently. In other words, one person may have plantar fasciitis despite having no heel spur, while another may have a heel spur but have no inflammation of the fascia or any heel pain.
How do you treat plantar fasciitis?
The initial treatment is rest, icing, stretching and nonsteroidal anti-inflammatories (NSAIDs) like ibuprofen. Massaging and stretching the foot, Achilles tendon and calf muscle helps relieve the tension on the plantar fascia. Physical therapy and/or orthotics and splints may also be used. In rare cases, surgery may be recommended.
In addition to resting, stretching, etc., many patients also find it helpful to roll a frozen water bottle under the foot. If the plantar fasciitis persists or worsens after rest, stretching and anti-inflammatory pain medications have been tried, a foot specialist might recommend:
- Physical therapy: Specific exercises and movements can help stretch and strengthen your feet and protect you from inflammation.
- A night splint: This holds the calf in a stretched position while you are resting.
- Orthotics: Custom orthotics can help with any anatomical issues while walking and exercising to distribute pressure more evenly.
- Corticosteroid injections: These may be injected into the most inflamed area of the foot and should ease the pain for about a month and decrease the amount of inflammation dramatically.
- Extracorporeal shock wave therapy – those who do not respond to physical therapy and other methods might be eligible for this nonsurgical technique that uses the same waves that break up kidney stones.
Is there surgery for plantar fasciitis?
About 95% of people with plantar fasciitis do not need surgery. It can take months or years to treat it successfully using nonsurgical means, and even then, it can reoccur. For those with very serious cases, there are surgical procedures to reduce tension on the fascia, including tenex and plantar fasciitis release.
- Tenex is a minimally invasive procedure that uses high-frequency vibrations and special instruments to remove scar tissue from the plantar fascia.
- Plantar fasciitis release. Either by open surgery or by endoscopic procedure with very small incisions, this is where the surgeon cuts part of the fascia to release tension and swelling.
As with any surgery, there are risks involved that your surgeon should go over before making the decision to have plantar fasciitis surgery.
What is the recovery time for plantar fasciitis surgery?
Recovery depends on the type of surgical procedure, but it usually takes up to 6 to 10 weeks. It may be about three months before you may return to rigorous activity.
