Treatment Options for Hip Pain
Non-surgical treatment should always be considered first when treating hip pain. With some conditions, it is possible to resolve the pain with rest, modifying one’s behavior, and a physical therapy and/or anti-inflammatory regimen. Such conservative treatments have been successful in reducing pain and swelling.
How to manage hip pain
If you find yourself with hip pain, it's important to consult a physician. An examination will help to determine what's causing the soreness, since hip pain can actually come from locations other than the hip, such as the spine, pelvis or leg. While waiting to see a physician, there are some modifications and exercises that may provide some relief.
Anti-inflammatories
Anti-inflammatories, commonly known as non-steroidal anti-inflammatory drugs (usually abbreviated as NSAIDs or NAIDs) are used primarily to treat mild to moderate pain associated with inflammation. This inflammation may be the result of muscular tears, bursitis, tendonitis, arthritis, labral tears, or synovitis. Anti-inflammatories are also used as a first line treatment in conjunction with a strengthening program. Post-operatively, they are prescribed as well.
Physical therapy
Physical therapy is an integral component to the multi-faceted team approach of examining and treating hip pain. The importance of physical therapy is to assist in gaining an understanding of the underlying causes of hip pain and then to collaborate with a team of physicians in order to design a comprehensive treatment approach. Rehabilitation is useful in many ways. It may be used as a non-invasive approach to treatment, whereby surgery for the patient is not or no longer indicated.
The hip joint is a very deep joint surrounded by almost 30 muscles. Physical therapy aims to strengthen these muscles, increase flexibility, maintain range of motion of the joint, and decrease the associated inflammation. In the case of a labral tear, physical therapy will not heal the tear. With the appropriate muscular training and activity modification, however, the condition may become asymptomatic and therefore require no surgery.
If operative treatment is inevitable, a pre-operative physical therapy program will provide the ability to address nearly all underlying joint problems or muscle imbalance, which ultimately leads to a better outcome. Additionally, in the event of surgery, post-operative therapy is essential in educating the patient regarding daily activities and in providing an appropriate recovery course. Physical therapy is an integral component in the management of hip pain.
Injections
Injections are commonly prescribed to help relieve a patient’s pain as well as to diagnose the direct cause of the pain.
Diagnostic
Following an injection of a numbing drug into the joint, immediate relief from pain will help confirm that the joint is the source of pain. If complete pain relief is achieved while the hip joint is numb, the joint is likely to be the source of pain. If not, further consideration of a possible cause is needed.
Pain Relief
- Intra-articular Injections is an ultrasound-guided cortisone injection made directly into the hip joint that can provide relief. Ultrasound-guided cortisone injections using dedicated high-resolution ultrasound equipment are very precise and allow a radiologist to target the injections directly into an area, maximizing therapeutic outcomes. Following the injection, pain relief varies from patient to patient. Some may feel relief from pain within two to five days. If a patient feels no relief within ten days following the injection, the patient is unlikely to gain any additional improvement and further diagnostic testing may be needed to identify other options for relief.
- Psoas Injection, which are performed under ultrasound, are often prescribed when the diagnosis is thought to be a symptomatic psoas tendon, which runs outside of the hip joint. In some cases, this diagnosis is difficult to make, as a painful psoas tendon often results in compression and tears of the labrum. As a result, pain relief following a psoas injection will only occur outside of the hip joint. If there is involvement of the labrum, which is inside the joint, additional evaluation is recommended.
- Trochanteric Bursa Injection injections is prescribed for patients who present clinically with bursitis on the outside of their hip, and for whom physical therapy and an anti-inflammatory regimen has not provided relief.
Hip arthroscopy
What is hip arthroscopy?
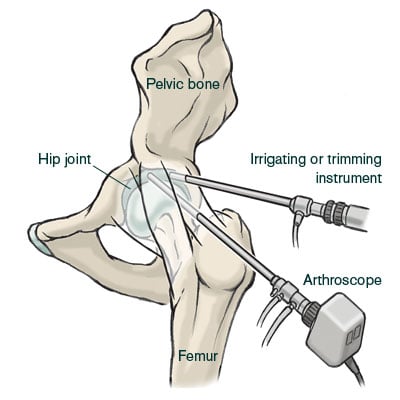
Recent advances in the development of surgical equipment have allowed orthopedic surgeons to treat conditions that were traditionally either ignored or treated with an open procedure. Now, with just a small incision, a surgeon can insert a pencil-sized optical device into the hip joint, which relays an image to a large video monitor in the operating room, allowing a surgeon to see into the joint and correct problems.
What happens during a hip arthroscopy?
Hip arthroscopy, or a “hip scope,” is a minimally-invasive procedure. The use of an arthroscope means that the procedure is done using 2-3 small incisions rather than a more invasive “open” surgery that would require a much larger incision. These small incisions, or “portals," are used to insert the surgical instruments into the joint. Occasionally, a third or fourth incision may be required depending upon the procedure. Excellent visualization of the entire joint is possible.
The patients are placed supine (on the back) and traction is applied under the guidance of fluoroscopy to allow for the placement of instruments. The amount of force needed to distract the hip varies from patient to patient, with every effort made to minimize the amount of traction. This practice decreases the amount of neuropraxia that develops post-operatively.
Through the second opening, surgical instruments are inserted to shave tissue, cauterize structures, or remove pieces. On occasion, holes may be drilled into patches of bare bone where the cartilage has been lost. This technique, called "microfracture" or "picking," provokes localized bleeding and encourages the formation of fibrocartilage (repair cartilage). Saline is pumped through the joint during the procedure to improve visualization and flush out debrided tissue. For more information, see Hip Arthroscopy.
Hip arthroscopy procedures
Synovectomy
When the inflamed synovial lining of the hip joint causes disabling pain, it may have to be removed via a synovectomy. By inserting heat-generating radio frequency probes inside the joint capsule, the inflamed tissue is then removed.
Treatment of labral tears
The location, chronicity, and vascularity of the injured fibrocartilage determine the way that labral tears are treated, with the goal of preserving as much healthy labral tissue as possible.
- Labral Debridement: If the quality of the labral tissue is poor, a debridement of the labrum is performed. This is done with the use of a rotating shaver in the joint that "trims" away involved tissue.
- Labral Refixation: If the quality of the labral tissue is adequate, an anchor is placed into the bone (acetabular rim). The suture attached to the anchor is then fed around the labral tissue and tied down to the acetabulum. This refixation procedure should make it possible for scar tissue to grow down the acetabulum and remain there once the suture dissolves.
- Partial Psoas Release: From inside the hip joint, the psoas tendon is brought into view by making a small window in the hip capsule. The lengthening of the tight tendon begins first, followed by a cut to release it, which allows the tendon to fill in with scar tissue, ultimately resulting in its lengthening.
Impingement procedures
- Acetabuloplasty (Rim Trimming/Decompression): Anterior over-coverage secondary to a pincer lesion can be treated arthroscopically. This lesion is usually associated with a flattened, degenerative or cystic labrum. Pincer lesions require bony resection, which can be performed using a motorized burr. Resection of the rim lesion oftentimes leads to destabilization or requires detachment of the labrum in order to fully visualize the extra bone. Following the rim resection, unstable, but healthy, residual labral tissue is refixed to the acetabular rim using arthroscopic suture anchoring techniques.
- Osteochondroplasty (CAM decompression): With visualization of the Cam lesion, a motorized burr is introduced and the removal of the Cam lesion is performed to recreate a spherical femoral head. A resection of less than 30% of the head neck junction is recommended to preserve the load bearing capacity of the femoral neck, and therefore decrease the risk of a stress fracture. Fluoroscopy is often used to assist in determining the amount of bone in need of resection.
Hip dysplasia procedures
- Osteotomy: The femur is surgically reshaped and repositioned to restore a more normal anatomy. This allows for normal hip motion and alleviates the impingement. Some osteotomies can be performed via minimally invasive procedures that use small incisions. An osteotomy that involves cutting the bone (and usually an open procedure, not an arthroscopic one) is a technique where the anatomy of the femur or socket is altered to relieve pain and prolong survival of the joint by reducing the abnormal loads on the cartilage. See animation below explaining periacetabular osteotomy (PAO):
- Arthrotomy: This is a procedure where the joint is opened to clean out bone spurs, loose bodies, tumors, or to repair fractures.
- Iliotibial Band (ITB) Release: An ITB release is performed in patients with symptomatic (painful) snaps. This is performed by accessing the lateral space in the hip. Once the ITB is visualized, a cut is made to lengthen the tissue.
- Trochanteric Bursectomy: A trochanteric bursectomy is a simple procedure in which a motorized shaver is placed in the peritrochanteric space (outside of the hip) to debride the inflamed bursal tissue.
- Gluteus Medius Repair: In the majority of cases, the procedure is completed arthroscopically; however, the size and/or location of the tear may warrant an open procedure. The tendons are visualized and an anchor(s) is placed into the greater trochanter of the femur while a suture is passed around the tendon. The tendon is then pulled down to its normal anatomic position and tied over the bone. The procedure is very similar to that of a rotator cuff in the shoulder.
- Removal of Loose Bodies/Tumors, (PVNS/Synovial Chondromatosis), Chondral Repair/Debridement, Chondroplasty: Performing a chondroplasty consists of removing loose fragments of cartilage, often associated with arthritis. The cartilage is taken out of the joint by a motorized shaver or a grasper depending upon the size of the fragments.
Hip arthroscopy and anesthesia
There are two options for anesthesia with arthroscopy: general or regional. Regional is the preferred option, as it allows for pain control immediately following surgery, and tends to minimize anesthetic side effects including, but not limited to, nausea, vomiting, pain at the site of insertion, spinal headache, and so on. Some patients that have spine pathology or bleeding disorders may not be candidates for a regional block. In this case, general anesthesia is recommended.
In the majority of hip arthroscopy cases, when a regional anesthesia is used, a spinal block is used rather than an epidural. A spinal block and epidural differ both in where the medication is administered into the spine as well as in the duration of its effect. For long cases, which will require an anesthesiologist to continually dose a patient over time, an epidural is warranted. For cases when a procedure should not exceed three hours, a spinal block is typically adequate. An anesthesiologist speaks with each patient prior to a procedure in order to make sure the patient is adequately informed. To learn more, read about Anesthesia Frequently Asked Questions.
Postoperative equipment
- Crutches: Crutch time varies, but is usually anywhere from 2-4 weeks. Gluteus medius repairs require 6 weeks on crutches, as does a microfracture procedure. Learn more about hip rehabilitation.
- Continuous Passive Motion (CPM) Machine: The CPM machine is a postoperative treatment method that is designed to aid recovery following joint surgery. For most recovering patients, attempts at independent joint motion causes pain and therefore the patient avoids moving the joint, which can lead to tissue stiffness around the joint and the formation of scar tissue. Ultimately, this may limit a patient’s range of motion and require physical therapy to restore the lost motion. The CPM machine moves the joint without the use of a patient’s muscles. The CPM machine is typically used for 4 hours/day for 4 weeks. A machine can be ordered through the Hip Preservation Service and can be delivered to the hospital on the day of surgery.
- Brace: A brace is worn for 2 weeks following surgery to prevent extreme flexion and extension of the hip, and is only worn during weight bearing activities using crutches. Due to the configuration of the brace, it must be worn over clothes. The brace, which is purchased through insurance, can be ordered by the Hip Preservation Service and delivered to the hospital on the day of surgery.
- Ice machine: The ice machine is a rented ice cooling system that is ordered by the Hip Preservation Service and delivered to the hospital on the day of surgery. It is to be used 4-6 times a day for 20-30 minutes at a time.
