How to Use Naloxone (Narcan) to Reverse an Opioid Overdose
What is naloxone (Narcan)?
Naloxone, more commonly known by the brand name Narcan, is a medicine used to reverse an opioid overdose by countering the effect an opioid has on your brain. Just as someone with allergies might carry an EpiPen (epinephrine injection device), or someone with diabetes may carry glucagon, naloxone is for emergency use and can save a person’s life. Studies show there are bystanders present during one out of three opioid overdose deaths.1 If more people carried naloxone for emergencies, many lives could be saved. Emergency medical services (EMS) data from Massachusetts found that 93.5% of people given naloxone survived their overdose.2
There are several types of naloxone delivery systems:
- nasal spray (generic naloxone, Narcan, Kloxxado)
- auto-injector – an automated, single dose injection delivered with a handheld device by pushing a button (Evzio, Zimhi)
- injection syringes (Prenoxad injection, Narcotan)
In this article, we will explain how to use Narcan, a brand of naloxone administered as a nasal spray. This is the type of naloxone that HSS dispenses as a certified distributor for the New York State Opioid Overdose Program.

Nalaxone (Narcan) nasal spray
Nalaxone (Narcan) auto-injector

Nalaxone (Narcan) injection
How does naloxone (Narcan) work?
Naloxone is an opiate antagonist – a medicine used to reverse opioid overdose by blocking opioids from binding to receptors in the brain.3 When naloxone is given by nasal spray or by an injection, the medicine knocks opioids out of receptors in the brain for a short time, giving the person a chance to breathe again.4 The family of opioid drugs on which naloxone works includes prescription pain medications such as oxycodone (OxyContin), fentanyl, hydrocodone (Vicodin), hydromorphone (Dilaudid), morphine, methadone, and illegal street drugs like heroin.
Who is at high risk for opioid overdose?
People at high risk of opioid overdose include those who:
- take high doses of opioids
- inject opioids into their body
- have pre-existing conditions
- mix opioids with other drugs, including illicit substances or benzodiazepines (such as Valium, Klonopin, Ativan, or Xanax)
It is important to know that it is possible to accidentally take more opioids than you realize, especially when taking illicit substances that might have fentanyl mixed with them. Fentanyl is a synthetic opioid that is up to 50 times stronger than heroin and 100 times stronger than morphine.5 It is a major contributor to overdoses in the United States, many of which are fatal. Fentanyl, especially illegally made fentanyl, is often mixed into illicit drugs to make them cheaper but more powerful. Because fentanyl is so potent, it also makes these drugs far more addictive and dangerous.
Fentanyl can come in powder, liquid, or tablet form. It is frequently mixed with drugs like heroin, cocaine, and methamphetamine, or made into pills that look like prescription opioids. In a liquid form, it can be taken with nasal spray, eye drops, or put onto paper or candies.
Many people selling or using drugs are not aware that their drugs are laced with fentanyl, or how much fentanyl is mixed into the drugs. It is possible for both first-time and long-term drug users to accidentally overdose. Any type of opioid overdose, whether prescription or illicit opioids, can lead to death. It should be noted that naloxone will not reverse the effects of non-opioid drugs with which fentanyl or any other opioid may be mixed (including cocaine and methamphetamines). It will only work on the opioids themselves.
When should you administer naloxone (Narcan)?
Naloxone should be administered to anyone you suspect may be having an opioid overdose. Naloxone works on opioids, including heroin, fentanyl, and prescribed opioid medicines. It does not work on non-opioid drugs such as benzodiazepines, cocaine, methamphetamines or alcohol. However, naloxone will not hurt someone who is not having an opioid overdose, so you can still administer naloxone if you are not sure what is causing the overdose.
What are the signs of an opioid overdose?
Signs of an opioid overdose include:
- a pale or clammy face
- small, constricted “pin-point” pupils
- limp body
- blue or purple fingernails or lips
- gurgling noises or vomiting
- difficult to wake or is unable to speak
- breathing or heartbeat slows or stops
How do you administer naloxone (Narcan)?
If you believe someone is having an opioid overdose, call 911 right away, then administer naloxone.
You can watch our naloxone (Narcan) training video6, or read the instructions below:
How to administer naloxone (Narcan)
Important note: There is only one dose in every applicator, so do not test it first!
Move the person onto their back, then follow the three Ps: Peel, Place and Press.
- Peel: Open the box, and peel back the paper.
- Hold the plunger with your thumb on the plunger and your index and middle fingers on either side of the nozzle.
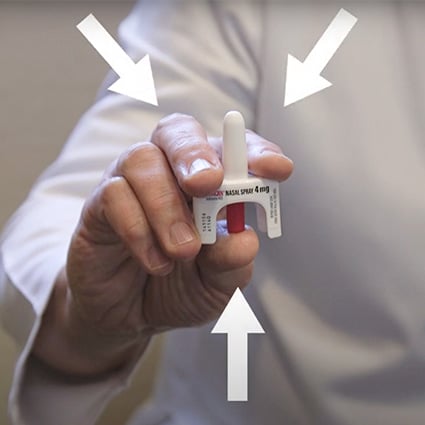
- Tilt the person’s head back and support their neck to open their airway.
- Hold the plunger with your thumb on the plunger and your index and middle fingers on either side of the nozzle.
- Place: Place the nozzle into one nostril as deep as it will go.
- Press: Press the plunger down all the way until your finger touches the person’s nose.
- Roll the person onto their left side.
- Stay with them until medical help arrives. Try to keep them awake and breathing.
- If they don’t wake up, you can give more doses of naloxone every two to three minutes. Multiple doses may be required because some opioids last longer in the brain than naloxone does.7
What are the side effects of naloxone?
Naloxone has little to no effects in most people who do not have opioids in their system, which is why it is often better to be safe than sorry. If you are not sure whether a person is overdosing from opioids, it usually best to administer naloxone anyway. Be sure to also call 911 right away.
For people who do have opioids in their system, naloxone may cause side effects such as:
- increased sweating
- nausea
- restlessness
- trembling
- vomiting
- flushing
- headache
Naloxone may also block natural endorphins created by the body that reduce pain. Other rare side effects may include:
- heart rhythm changes
- seizures
- pulmonary edema (fluid accumulation in the lungs)
Naloxone can also cause other adverse events, including:
- Other cardiovascular effects (hypertension, hypotension, tachycardia, ventricular fibrillation, ventricular tachycardia).
- Central nervous system effects, such as agitation, body pain, brain disease, and coma.
- Cases of allergy or hypersensitivity. Naloxone is contraindicated in people with hypersensitivity to naloxone or any of its formulation components.
Naloxone should be used with caution in people who:
- Have cardiovascular disease.
- Are currently taking medications that could have adverse effects on their cardiovascular system, including low blood pressure, pulmonary edema, and abnormal heart rhythms. There have been reports of opioid antagonists leading to pulmonary edema and ventricular fibrillation.8
What is the difference between naloxone and naltrexone?
Naloxone is an emergency treatment that can reverse opioid overdose, and it can often be acquired over the counter without a prescription. Naltrexone is not an emergency medicine – it is a substance use treatment prescribed by a doctor.9 Naltrexone is taken either as pills or an injection, and it blocks opioids and alcohol from providing the “high” feeling that people get from using these substances. However, it doesn’t actually stop you from being intoxicated, even if you don’t feel drunk or high. Do not drive or do anything that requires you to be mentally alert.
How can I get naloxone (Narcan)?
In most states, you don’t need a prescription to get naloxone from a pharmacy. Ask your doctor or pharmacist about getting naloxone.
In New York state, you may be eligible for the Naloxone Co-payment Assistance Program (N-CAP), which can help reduce the cost of naloxone.10 Other states also have naloxone awareness programs, so check to see what programs exist in your state.
If you are having surgery at HSS, you can ask about getting a naloxone (Narcan) kit for free from HSS. HSS is a certified distributor for the NYS Opioid Overdose Program. The chronic pain service has naloxone kits available for patients in the hospital.
References
- Naloxone. Centers for Disease Control and Prevention. 2012 Apr 21. Retrieved from https://www.cdc.gov/stopoverdose/naloxone/index.html.
- Nadia Kounang. Naloxone reverses 93% of overdoses, but many recipients don’t survive a year. CNN.com. 2017 Oct 30. Retrieved from https://edition.cnn.com/2017/10/30/health/naloxone-reversal-success-study/index.html.
- Narcanti. Minimally Invasive Neurosurgery Clinic. 2022 Jan 23. Retrieved from https://www.minclinic.ru/drugs/drugs_eng/N/Narcanti.html.
- Opioid Overdose Basics: Understanding Naloxone. The Harm Reduction Coalition. 2020 Sep 8. Retrieved from https://harmreduction.org/issues/overdose-prevention/overview/overdose-basics/understanding-naloxone/.
- Centers for Disease Control and Prevention. Fentanyl Facts. 2023 Jun 27. Naloxone. Retrieved from https://www.cdc.gov/stopoverdose/fentanyl/index.html.
- Seth A. Waldman, MD. How to Use Naloxone | Reversing an Opioid Overdose. Hospital for Special Surgery. 2022 Jul 6. Retrieved from https://www.youtube.com/watch?v=mraqEbCYlFY&list=PLDps2oOp60a76hl1hDyd0u_pCENgo3dL8&index=6.
- Naloxone (Monograph). American Society of Health-System Pharmacists. 2023 Mar 30. Retrieved from https://www.drugs.com/monograph/naloxone.html.
- Naloxone Hydrochloride. Hospira, Inc. 2019 Sep. Retrieved from https://labeling.pfizer.com/ShowLabeling.aspx?id=4541.
- Marijke Vroomen Durning, RN. Naloxone vs. Naltrexone. WebMD. 2022 Apr 29. Retrieved from https://www.webmd.com/mental-health/addiction/naloxone-vs-naltrexone.
- Availability of Naloxone in Pharmacies. New York State Department of Health. 2023 Feb. Retrieved from https://www.health.ny.gov/diseases/aids/general/opioid_overdose_prevention/directories.htm.


