The Use of Autoantibody Testing in a Postpartum Patient at Risk of Malignancy-Associated Dermatomyositis
From Grand Rounds from HSS: Management of Complex Cases | Volume 9, Issue 2
Case Report
In May 2019, a 32-year-old woman developed a rash on her face, chest, and knuckles, initially thought to be contact dermatitis. She saw a second dermatologist to evaluate persistent symptoms, who found positive results on antinuclear antibody (ANA) testing. She was referred to rheumatology, but additional lab testing was unrevealing. She learned she was pregnant, and the rash resolved spontaneously 4 weeks into the pregnancy. She delivered a heathy son at 40 weeks’ gestation. Approximately 8 weeks postpartum, the rash on her face, chest, and knuckles recurred. About 4 and a half months postpartum, she developed fatigue and weakness of her proximal arms and legs, and came to HSS for evaluation. She had no shortness of breath or dysphagia.
The patient had a prior uncomplicated pregnancy, no prior surgeries, and no family history of autoimmunity but did have a first-degree relative with a BRCA mutation. She was breastfeeding and planned to wean in the setting of possibly needing additional medications. She was married, with 2 young children, and worked full-time.
Her physical exam was notable for erythema of her cheeks and upper chest and erythematous papules over the meta-carpophalangeal joints consistent with Gottron’s papules. She could not abduct her shoulders above 90° against gravity, although she could stand from a seated position without using her arms.
Laboratory testing showed a white blood cell count of 3.3 cells/mm3 and elevated levels of aspartate aminotransferase (45 U/L), creatine kinase (CK, 665 U/L), aldolase (10.6 U/L), and lactate dehydro-genase (LDH, 324 U/L). An ANA test was positive in a speckled pattern at a 1:320 dilution, while tests of anti-Jo-1, anti-RNP, and anti-dsDNA antibodies were negative, complement C3 and C4 were normal, and erythrocyte sedimentation rate was normal. Myositis autoantibody profiling was positive for p155/140 (TIF-1γ). A skin biopsy result was consistent with dermatomyositis (Fig. 1). Pulmonary function testing and echocardiography were normal.
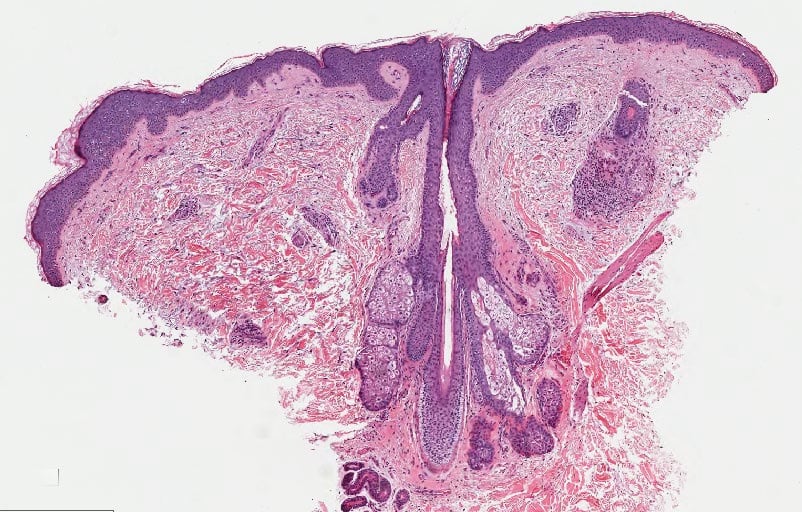
Figure 1a: Hematoxylin and eosin staining of biopsy demonstrates dermatomyositis.
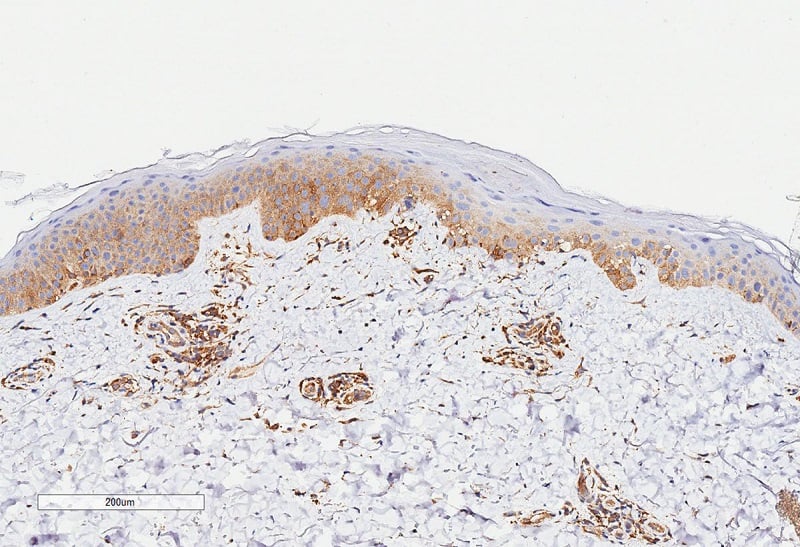
Figure 1b: MxA staining, which binds to endothelial cells.
She was started on high-dose prednisone, with rapid, significant partial improvement in strength and skin disease. Azathioprine 50 mg daily was then added. Over the next several weeks, her strength continued to improve and the rash to fade, and CK and LDH levels fell. Intravenous immunoglobulin (IVIG) 2g/kg monthly was added for additional steroid sparing and symptom control, and she noted further skin improvement. A second series of IVIG doses was unfortunately associated with development of aseptic meningitis requiring hospitalization.
Malignancy screening was performed. Computed tomography (CT) scanning of the chest/abdomen/pelvis was normal. Esophagogastroduodenoscopy and colonoscopy revealed features of celiac disease and lymphocytic colitis. Mammography showed changes consistent with lactation. Genetic testing disclosed no BRCA 1/2 mutations but did show a mutated checkpoint kinase 2 (CHEK2) allele, which is associat-ed with an increased risk of ovarian, colon, and breast cancer.
Discussion
Pregnancy outcomes in myositis are variable, but generally good outcomes are associated with good disease control prior to pregnancy, as in other rheumatic diseases such as lupus [1]. It has long been recognized that a subset of patients with rheumatoid arthritis do particularly well during pregnancy, achieving reduced disease activity, or even remission, though they may flare again postpartum. Our case demonstrates this spontaneous improvement phenomenon manifesting in dermatomyositis, which has been described in a small Spanish case series [2] but is nonetheless very rare.
Anti-TIF-1γ antibodies are specific to patients with dermatomyositis, most commonly patients with malignancy-associated dermatomyositis. In a recent large study, 38% of patients positive for anti-TIF-1γ developed cancer, versus 15% of patients who were anti-TIF-1γ negative [3]. While our patient did not exhibit signs of malignancy after comprehensive screening, the risk of an occult malignancy emerging remains elevated in patients with anti-TIF-1γ for 3 years after dermatomyositis disease onset [3]. Ongoing screening is merited over that period in these patients. However, the risk of malignancy in this context is also tightly related to age. Juvenile dermatomyositis poses essentially no risk of malignancy, and malignancy risk remains low but not nonexistent in those under 40 years of age [3,4]. Our patient will continue with intensive lifelong screening for malignancy based on the presence of a heterozygous mutation in the tumor suppressor gene CHEK2, which has been implicated in increased risk of several cancers, including breast cancer [5].
This case illustrates several interesting features of rheumatic disease during pregnancy, as well as the use of autoantibody testing to identify patients at high risk of malignancy-associated dermatomyositis, who would benefit from more prolonged surveillance.
References
- Munira S, Christopher-Stine L. Pregnancy in myositis and scleroderma. Best Pract Res Clin Obstet Gynaecol. 2020;64:59-67.
- Iago PF, Albert SOC, Andreu FC, et al. “Pregnancy in adult-onset idiopathic inflammatory myopathy”: Report from a cohort of myositis patients from a single center. Semin Arthritis Rheum. 2014;44(2):234-240.
- Oldroyd A, Sergeant JC, New P, et al. The temporal relationship between cancer and adult onset anti-transcriptional intermediary factor 1 antibody-positive dermatomyositis. Rheumatol (United Kingdom). 2019;58(4):650-655.
- Fiorentino DF, Chung LS, Christopher-stine L, et al. Most patients with cancer-associated dermatomyositis have antibodies to nuclear matrix protein NXP-2 or transcription intermediary factor 1. Arthritis Rheum. 2013;65(11):2954-2962. 3
- Apostolou P, Papasotiriou I. Current perspectives on CHEK2 mutations in breast cancer. Breast Cancer Targets Ther. 2017;9:331-335.


