Scoliosis Treatment for Adults
Scoliosis most commonly appears during childhood or adolescence, but it can also develop and progress during adulthood.
What is scoliosis?
Scoliosis is a lateral (or sideways) curvature of the spine in one or more places. This is different from the condition known as kyphosis, where the spine has an abnormal, forward-oriented curvature. Scoliosis and kyphosis often occur together.
What is adult scoliosis?
Scoliosis most frequently occurs in children and teenagers. However, adults may also be diagnosed with scoliosis, either when a curve that existed in their youth progresses, or as a de novo (newly diagnosed condition) that can result from degenerative changes in the spine, accompanied by stenosis and osteoporosis.




Figures 1-4: Progression of adult scoliosis from age 14 (top left) to age 46 (lower right).
What part of the spine curves in people with scoliosis?
Scoliosis can affect the spine in any of its three major sections:
- cervical spine (neck)
- thoracic spine (chest and upper back region)
- lumbar spine (lower back)
Imbalances in the above can result also in lower extremity imbalance in the hips, knees and ankles.
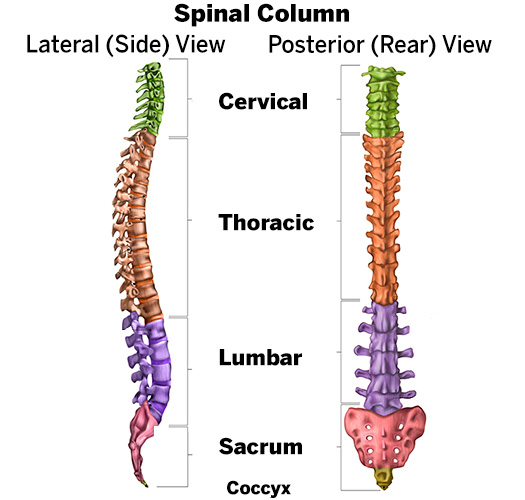
Figure 5: Diagram showing the sections of the healthy spine, with the neck (cervical) section at the top, followed below by the thoracic and lumbar sections, the sacrum and the coccyx (tailbone). The curvature shown in the left image is the normal curve of the spine when it is viewed from the side (not scoliosis).
What are the symptoms of scoliosis in adults?
The most common symptoms of scoliosis in adults are pain and, often, a visible bulge on the back at the site of this pain. Less often, people may experience fatigue, a loss of height, or a feeling of fullness when, in fact, the stomach is empty. It is also common to have referred pain in the leg pain due to spinal stenosis at the apex of the scoliosis curve.
Common symptoms
- Pain: Adults with scoliosis often experience pain, which leads them to seek medical care. Pain may be related to the curve itself or due to compression of the spinal nerves. In some cases, there is also muscular fatigue related pain due to muscles on the convex side working harder to maintain postural balance while the concave muscles are mechanically disadvantaged to function optimally. This results in fatigue and failure especially after activities on the convex side. When there is nerve compression, this is called spinal stenosis. Stenosis can generate inflammation in nerves which, in turn, causes leg pain and numbness or weakness when walking or standing for a long period of time.
- Bulge or deformity in the back: Patients are usually able to point to the site of their back pain, and a bulge may be visible due to muscle rotation or rib cage rotation. Asymmetry in the trunk as it relates to the pelvis may be pronounced. There may also be an inability to stand upright.
Additional symptoms experienced by some adults with scoliosis
- Loss of height (stature).
- Shortness of breath or quick fatigue. This affects patients with large and progressive curves (over 70 degrees) that compress the lungs.
- Premature feeling of fullness in the stomach (hunger satiety). This affects people with progressive, thoracolumbar curves (curves that span the thoracic and lumbar sections of the spine). Associated pressure on the abdomen can make a person feel full while eating, even though the stomach itself is not truly full.
How is adult scoliosis diagnosed?
The medical evaluation for scoliosis includes:
- A physical exam.
- X-rays or low-dose radiation EOS imaging taken from the front and side views while the patient stands upright, to accurately measure the degree of the curve.
- X-rays or low-dose radiation EOS imaging taken while the patient bends over in order to assess the flexibility of the curve.
- X-rays taken in a supine position in order to assess flexibility of the scoliosis.
Scoliosis is diagnosed when the curve exceeds 10 degrees. However, by the time adults seek treatment, the curve usually exceeds 30 degrees.
The doctor will also use the physical exam and imaging to assess the patient for signs of spinal stenosis (the narrowing or compression of the spinal canal). Additional tests may be ordered if there is evidence that the patient's lung function (breathing) is being affected by the scoliosis. In rare cases, patients with a severe scoliosis deformity may develop pulmonary heart disease, which will require evaluation and treatment by additional medical specialists.
The effects of the scoliosis on patient ADLs (activities of daily living) and quality of life are extremely important to consider when deciding on appropriate treatment options. Especially important is to provide an intervention that will best preserve a person’s functional status and participation in activities that the patient considers important for themselves. Whether it be walking, hiking, skiing, tennis, golf, swimming, surgical intervention should consider all of these before deciding on a specific surgical treatment option. This information also helps guide treatment choices.


Figures 6-7: Photo and X-ray of patient with severe curve progression and restrictive pulmonary disease.
How is scoliosis in adults treated?
Whenever possible, scoliosis in adults is treated non-operatively through physical therapy, medications and other methods. Steroid injections may also help some patients. Surgery may be warranted in patients who have curves that exceed 50 degrees, are not responding to nonsurgical methods or experience other complications. (Find a doctor at HSS who treats scoliosis.)
Nonsurgical treatments
Many patients experience significant relief of their pain from non-operative measures that may include:
- pain medication such as NSAIDs (nonsteroidal anti-inflammatory drugs)
- physical therapy to increase core muscle strength
- postural training
- weight maintenance
- activity modification
Patients who continue to experience nerve pain may benefit from steroid injections in the facet joints (where the vertebrae meet at each level of the spine). Steroids, which reduce inflammation, may also be administered by an epidural, in which the injection needle is inserted into the spinal canal to deliver the drugs directly to the affected nerve root.
In some patients experiencing muscle spasms, the doctor may prescribe a brace to be worn on a short-term basis. However, their usefulness is limited since the support they provide gradually weakens the muscles in the trunk and spine.
Surgical treatments
Surgery may be recommended for selected patients, including those who:
- do not respond to non-operative treatment after a period of time
- have curves that exceed 50 degrees and have significant impairment of daily function
- experience worsening lung or neurologic function.
- inability to stand upright to perform activities of daily living
The most common type of surgery in adults is a posterior spinal fusion with instrumentation (artificial implants). In this procedure, the orthopedic surgeon makes an incision from the back, places screws to correct the scoliosis and then essentially "welds" the vertebrae together using bone chips.
These chips may be:
- autografts – taken from elsewhere in the patient's own body
- allografts – sourced from donors through a bone bank.
The healing process used to take six months to one year or longer, although the recovery from surgery itself is usually 4 to 6 weeks. However, modern techniques and research done here at HSS have shortened the recovery times possible to 3 to 6 months. Rods, screws or other implants may be used to hold the spine in alignment during this period. Once the fusion is complete, these implants no longer serve a function but are left in place to avoid the need for additional surgery.
Depending on the nature of the curve and its location, the orthopedist may need to perform a fusion from both the front and the back of the body, a procedure that may be done as a single operation or in stages.



Figures 8-10: Pre-op images of an adult with lumbar scoliosis.



Figures 11-13: The same patient after anterior/posterior (front/back) spinal fusion and instrumentation.
Adults with very large and rigid curves may also require osteotomies, in which stiff segments of the facet joints are released.
Some patients with lumbar and thoracolumbar curves may be candidates for thoracoscopic or lateral assess surgery, in which incisions are made from the side of the torso or flank. As with the posterior and anterior approaches, instrumentation corrects the curve and the rotation of the spine.
Adults with scoliosis and spinal stenosis often also require a decompression procedure in which the roof of the vertebral column is removed at the affected area, freeing the nerve from any material that is compressing it, prior to fusion.
Whenever surgery is considered, the orthopedic surgeon reviews the risks and benefits with the patient, taking into account the person's age and medical history. The presence of other conditions can pose additional surgical challenges, including:
- arthritis
- kyphosis (a forward curvature of the spine)
- osteoporosis (a condition in which bone density decreases and the bones become more fragile and likely to break on impact)
- Other, non-orthopedic, medical conditions
To address these challenges, surgeons at HSS work with a multidisciplinary team of:
- internists (internal medicine physicians)
- pulmonologists
- neurologists
- anesthesiologists
- metabolic bone specialists (usually an endocrinologist or rheumatologist with specialized metabolic bone training)
- orthopedic nurses
Surgical patients are given antibiotics to help guard against infection, and their sensory and motor function is monitored throughout surgery to detect any changes in spinal code integrity during spinal manipulation and curve correction.
Surgical outcomes
In appropriately selected and prepared patients, surgical treatment has been shown to be superior to conservative measure for management with recent data suggesting sustained durability of benefit over 10 years. Correction of the curve falls in the range of 50% to 90%. The SRS 22 patient questionnaire, Oswestry Disability Index (ODI) and PROMIS scores help to quantify the level of pain relief and improvement of quality of life for each patient.
Complications of scoliosis surgery in adults can include:
- pseudarthrosis (a nonunion of the spine fusion), which may lead to loosening of the implanted instruments
- infections
- neurological problems
- blood clots
- spinal imbalance, which refers to problems with the correction, including the inability of unfused segments to spontaneously correct and balance the spine
Following surgery, most patients remain in the hospital for 1 to 5 days – or slightly longer for those who undergo combined anterior and posterior (front and back) surgery. They are usually back on their feet on the first day and walking with the physical therapists in the hospital.
Pain medication is continued as needed. As recovery progresses, patients are advised to limit their activities to walking and to avoid bending and heavy lifting for the first four weeks. By adhering to these guidelines and with the help of physical therapy, the patient should be able to resume normal activities at home by about four to six weeks. Those with desk jobs may return to work. Adults may take 3 to 6 months to achieve full functional recovery, and it is rare for adults to require pain medication for ongoing discomfort.
Patients should be aware that spinal fusion does result in some loss in range of motion; however, the degree varies depending on the site and length of the fusion. If the treatment is primarily in the thoracic spine, normal mobility is achieved after the healing process is completed. If the lumbar spine is the site of treatment, sideways movement will be more restricted, although the patient will still be able to bend forward from the hips. Similarly, fusion in the cervical spine places more restriction on movement.
While surgical treatment of scoliosis in adults can present a complex set of challenges, a team approach and the use of refined surgical techniques and instruments both help ensure a positive outcome. In addition, orthopedic surgeons are increasingly using bone morphogenic proteins (BMPs) in spinal fusions. These substances enhance and accelerate healing for a good long-term result.
Updated: 4/5/2025
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Professor of Orthopedic Surgery, Weill Cornell Medical College
Related articles
References
- Daniels AH, Singh M, Daher M, Balmaceno-Criss M, Lafage R, Gupta MC, Gum JL, Hamilton KD, Passias PG, Protopsaltis TS, Kebaish KM, Lenke LG, Ames CP, Klineberg EO, Kim HJ, Shaffrey CI, Smith JS, Line BG, Schwab FJ, Bess S, Lafage V, Diebo BG. Fractional curve following adult idiopathic scoliosis correction: impact of curve magnitude on postoperative outcomes. J Neurosurg Spine. 2024 Nov 15;42(2):193-202. doi: 10.3171/2024.7.SPINE24519. PMID: 39546796. https://pubmed.ncbi.nlm.nih.gov/39546796/
- Mullin JP, Quiceno E, Soliman MAR, Daniels AH, Smith JS, Kelly MP, Ames CP, Bess S, Burton D, Diebo B, Eastlack RK, Hostin R, Kebaish K, Kim HJ, Klineberg E, Lafage V, Lenke LG, Lewis SJ, Mundis G Jr, Passias PG, Protopsaltis TS, Schwab FJ, Gum JL, Buell TJ, Shaffrey CI, Gupta MC; International Spine Study Group. Comparison of clinical and radiological outcomes of three-column lumbar osteotomies with and without interbody cages for adult spinal deformity. Spine J. 2025 Jan 10:S1529-9430(25)00019-1. doi: 10.1016/j.spinee.2025.01.001. Epub ahead of print. PMID: 39800321. https://pubmed.ncbi.nlm.nih.gov/39800321/
- Passias PG, Tretiakov P, Onafowokan OO, Das A, Lafage R, Smith JS, Line BG, Nayak P, Diebo B, Daniels AH, Gum JL, Hamilton DK, Buell TJ, Soroceanu A, Scheer JK, Eastlack RK, Mullin JP, Schoenfeld AJ, Mundis GM, Hosogane N, Yagi M, Mummaneni PV, Chou D, Fu KM, Than KD, Anand N, Okonkwo DO, Wang MY, Klineberg E, Kebaish KM, Lewis S, Hostin R, Gupta M, Lenke L, Kim HJ, Ames CP, Shaffrey CI, Bess S, Schwab F, Lafage V, Burton D. When is staging complex adult spinal deformity advantageous? Identifying subsets of patients who benefit from staged interventions. J Neurosurg Spine. 2024 Nov 22;42(2):185-192. doi: 10.3171/2024.8.SPINE24365. PMID: 39576989. https://pubmed.ncbi.nlm.nih.gov/39576989/
- Smith JS, Ben-Israel D, Kelly MP, Lafage V, Lafage R, Klineberg EO, Kim HJ, Line B, Protopsaltis TS, Passias P, Eastlack RK, Mundis GM, Riew KD, Kebaish K, Park P, Gupta MC, Gum JL, Daniels AH, Diebo BG, Hostin R, Scheer JK, Soroceanu A, Hamilton DK, Buell TJ, Lewis SJ, Lenke LG, Mullin JP, Schwab FJ, Burton D, Shaffrey CI, Ames CP, Bess S. The gap between surgeon goal and achieved sagittal alignment in adult cervical spine deformity surgery. J Neurosurg Spine. 2025 Jan 3:1-11. doi: 10.3171/2024.8.SPINE24703. Epub ahead of print. PMID: 39752660. https://pubmed.ncbi.nlm.nih.gov/39752660/
- Smith JS, Kelly MP, Yanik EL, Baldus CR, Pham V, Ben-Israel D, Lurie JD, Edwards C, Glassman SD, Lenke LG, Buchowski JM, Carreon LY, Crawford CH 3rd, Lewis SJ, Koski T, Lafage V, Gupta MC, Kim HJ, Ames CP, Bess S, Schwab FJ, Shaffrey CI, Bridwell KH. Operative vs Nonoperative Treatment for Adult Symptomatic Lumbar Scoliosis at 8-Year Follow-Up: A Nonrandomized Clinical Trial. JAMA Surg. 2025 Apr 2. doi: 10.1001/jamasurg.2025.0496. Epub ahead of print. PMID: 40172880. https://pubmed.ncbi.nlm.nih.gov/40172880/