Spondylolysis (Pars Fracture)
Spondylolysis is a stress fracture of the spine that is common in young athletes, especially in those who repeatedly bend backwards during activity, such as gymnasts.
What is spondylolysis?
Spondylolysis is a spinal defect or fracture of a bone structure called the pars interarticularis, which connects the facet joints of the spine. The condition is sometimes also called by the shortened names, “pars defect” or "pars fracture."
The spinal cord is protected by rings of bone that make up the middle and posterior (rear) portion of the spinal column. In each of these rings, the pars interarticularis (or simply "pars" for short), located on each side of the vertebra, connects other components of the ring, known as the pedicle and lamina.
Illustration of the spinal column and location of a pars fracture (spondylolysis)
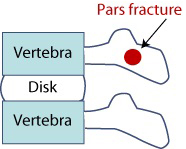
Figure 1: Side view of spinal column
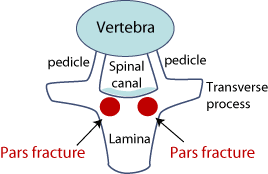
Figure 2: Top view of spinal column
What causes spondylolysis?
Spondylolysis usually occurs during childhood or adolescence from repetitive stress, rather than from an acute injury. In other words, it is usually a stress fracture rather than a sudden break. These stress fractures in the back are most often seen in adolescent athletes such as gymnasts, where there is a great deal of extension and landing with an arched back. Spondylolysis is the most common cause of structural back pain in children and teenagers.
Spondylolysis is a common condition of children and teenagers who are involved in organized sports. Active kids and teens with spondylolysis may experience symptoms, however, some people with this condition may not develop symptoms until later in adulthood.
Where in the spine is spondylolysis most common?
Pars fractures most commonly occur in the lowest lumbar vertebra (L5) of the lower back (lumbar spine). In athletes, this type of injury can be seen when the back is bent backwards repeatedly, in activities such as gymnastics, karate and other martial arts. It is also common in soccer, lacrosse and basketball players. In football players, it is especially common in offensive and defensive linemen.
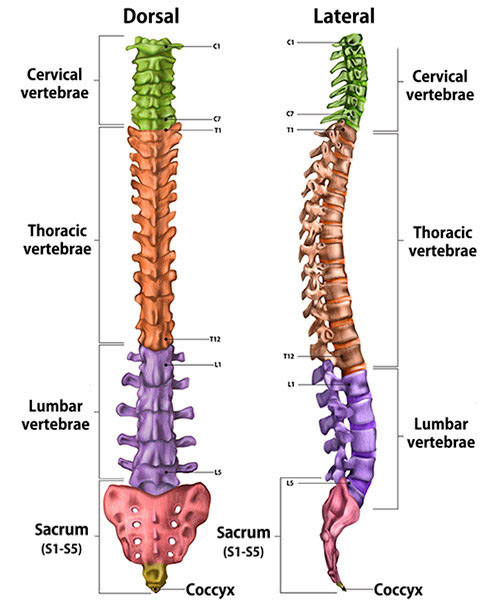
Illustration of cross-section of spine, dorsal (back to front) and lateral (side) views, showing its vertebral sections.
The vertebra initially responds to increased physical strain of such activity by gradually adding new bone cells around the stressed area of the spine. However, an injury can occur too quickly for the vertebra to be repaired, and this leads to a crack in the pars. The crack may affect only one side, but it is not uncommon to have fractures on both sides of the vertebra. When fractures occur on both sides, it is possible for one vertebra to translate or move forward or backward over the neighboring vertebra. This is called spondylolisthesis.
What are the symptoms of spondylolysis?
A person with a pars defect may feel pain and stiffness in the lower back that is worsened with activity and improves with rest. Hyperextension (abnormal stretching) of the lower back will usually aggravate the area as it overloads the pars fracture.
Occasionally, nerve symptoms can be present. These may include:
- a “pins and needles” sensation in a leg, with or without numbness or weakness in the leg
- pain in the back, neck, legs, thighs or shoulder
- muscle spasms or weakness
- tingling, numbness and/or stiffness in the back
How is spondylolysis diagnosed?
Evaluation for this condition includes a review of the patient’s medical history and a physical exam, followed by X-rays, which can detect a pars fracture. A CT scan may be used to evaluate a pars defect and to visualize healing bone, while an MRI may be useful to assess the surrounding tissue and condition of the disc.
How is spondylolysis treated?
The initial treatment for these types of stress fractures is rest from activity and bracing, followed by physical therapy. Treatment is individualized depending on the injury, age and the demands of the sport. The fracture can be assessed with a series of X-rays every few months. If the patient has persistent pain after nonsurgical treatment, surgery may be required.
When do I need surgery for spondylolysis?
Fortunately, the symptoms of spondylolysis almost always respond favorably to physical therapy and activity modification. In some instances, however, there may be persistent symptoms that necessitate surgical intervention. This usually occurs when one or more vertebrae slip out of place relative to one other (spondylolisthesis) or if there is persistent back pain.
In these cases, surgical options usually include lumbar spinal fusion or direct repair of the fracture. If there is pinching of a nerve associated with a spondylolysis, a laminectomy (spinal decompression surgery) may also be considered.
What is the recovery time for spondylolysis?
The recovery period for nonsurgical treatment ranges from a couple of weeks to several months depending on the severity. Recovery for surgical treatment depends on which particular spine surgery is appropriate.
Bracing can last for three to four months while the fracture heals, and physical therapy can also be included to maintain and help strengthen the abdominal and back muscles with specific directed exercises.
Articles on spondylolysis
Updated: 9/7/2022
Reviewed and updated by Sravisht Iyer, MD
References
- Ibiebele A, Scott D, D'Hemecourt P, Meehan WP 3rd. The use of bracing in the management of lumbar spondylolysis. PM R. 2022 May;14(5):604-610. doi: 10.1002/pmrj.12756. Epub 2022 Feb 23. PMID: 35014189.
- Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009 Apr;37(4):768-75. doi: 10.1177/0363546508329542. Epub 2009 Feb 19. PMID: 19229045.
- Hanke LF, Tuakli-Wosornu YA, Harrison JR, Moley PJ. The Relationship Between Sacral Slope and Symptomatic Isthmic Spondylolysis in a Cohort of High School Athletes: A Retrospective Analysis. PM R. 2018 May;10(5):501-506. doi: 10.1016/j.pmrj.2017.09.012. Epub 2017 Oct 6. PMID: 28993288.
- Kim HJ, Green DW. Adolescent back pain. Curr Opin Pediatr. 2008 Feb;20(1):37-45. doi: 10.1097/MOP.0b013e3282f357fe. PMID: 18197037.
- Kim HJ, Green DW. Spondylolysis in the adolescent athlete. Curr Opin Pediatr. 2011 Feb;23(1):68-72. doi: 10.1097/MOP.0b013e32834255c2. PMID: 21150440.
- Ladenhauf HN, Fabricant PD, Grossman E, Widmann RF, Green DW. Athletic participation in children with symptomatic spondylolysis in the New York area. Med Sci Sports Exerc. 2013 Oct;45(10):1971-4. doi: 10.1249/MSS.0b013e318294b4ed. PMID: 23559123.S


