Shoulder Replacement

Total shoulder replacement is a highly successful procedure to reduce pain and restore mobility in patients with end-stage shoulder arthritis and, in some cases, after a severe shoulder fracture. Shoulder replacement surgery relieves pain and helps restore motion, strength and function of the shoulder.
One year after surgery, 95% of patients have pain-free function, enabling them to exercise the shoulder to restore strength and motion. Most patients are able to return to playing golf or tennis, swimming, doing yoga or pilates, and other physical activity they previously avoided because of shoulder pain.
What is shoulder replacement surgery?
Total shoulder replacement, also known as total shoulder arthroplasty, is the removal of portions of the shoulder joint, which are replaced with artificial implants to reduce pain and restore range of rotation and mobility. It is very successful for treating the severe pain and stiffness caused by end-stage arthritis.
The primary joint of the shoulder, called the glenohumeral joint, is a ball-and-socket joint in which the humeral head (at the top of the humerus, or the upper arm bone) forms the ball and the glenoid cavity (at outer edge of the scapula, or shoulder blade.) forms the socket. The ball and socket are covered with smooth cartilage to facilitate gliding motion.
In arthritis of the shoulder, this smooth cartilage degenerates, causing the the bones surfaces to come into direct contact. This increases friction, which then damages and roughens the bone, causing stiffness and pain. Surgically implanted artificial replacement surfaces restore pain-free movement, strength and function.
What conditions are treated by shoulder replacement surgery?
Shoulder replacement is sometimes used to treat fractures that cause severe damage to the shoulder, but its primary use is to treat shoulder arthritis. There are two basic types of arthritis that affect the shoulder: osteoarthritis and inflammatory arthritis.
- Osteoarthritis is physical wear and tear on the cartilage inside the joint that develops from years of use. Although many older adults experience OA at some point, they are more likely to get it in their knees, hips or fingers than the shoulder. Osteoarthritis in the shoulder is more common in exceptionally active people (even at younger ages), such as tennis players, weightlifters and other athletes who put continual pressure on their shoulders. In some cases, a severe, acute injury triggers or contributes to this long-term damage, for example, a past torn rotator cuff or shoulder fracture
- Inflammatory arthritis is an umbrella term for several chronic, autoimmune diseases which have no completely understood cause. The two types of inflammatory arthritis that affect the shoulder are rheumatoid arthritis and ankylosing spondylitis. Many people with these conditions who have replacement surgeries experience reduced pain and improved function in the shoulder. (Some ankylosing spondylitis patients may also benefit from elbow replacement.)
How do I know if I need a shoulder replacement?
The most common reason for a person to have this surgery is when they have shoulder pain from arthritis that can't be controlled with nonsurgical treatments. The pain is usually accompanied by a progressive stiffness and a grinding or grating sensation in the shoulder.
These symptoms indicate that bones that form the ball and socket of the shoulder joint are rubbing against one another because the cartilage that should lie between them has worn away.
Diagnosing conditions that may be treated with a shoulder replacement
To diagnose arthritis in the shoulder, a doctor will order a series of standard X-rays. A CT scan may also be necessary to evaluate a patient's bone integrity, and magnetic resonance imaging (MRI) may be ordered to determine the condition of important surrounding soft tissues, such as the rotator cuff tendon.
If the doctor suspects there may be nerve damage, based discussions with the patient, an EMG test or nerve conduction study may be ordered to evaluate the nerves that feed the important muscles of the shoulder.
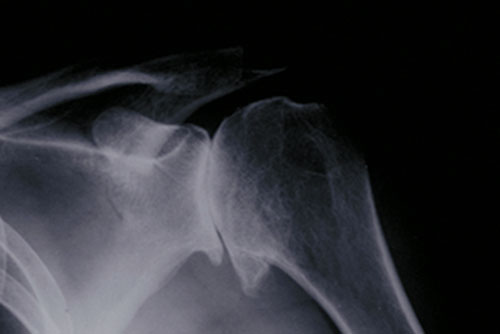
Figure 1: X-ray showing osteoarthritis of the shoulder joint, in which bones of the shoulder joint are in direct contact.
Who should not get a shoulder replacement?
Certain patients are not good candidates for shoulder replacement. These include those who:
- have symptoms that are not significantly disabling
- experience loss or paralysis of both rotator cuff and deltoid muscles
- have active infections
- have a progressive disease of the nervous system that has affected the joint (assessed on a case-by-case basis)
In addition, some patients who are experiencing early stage osteoarthritis may wish to first try nonsurgical, conservative management of their condition to determine whether a shoulder replacement is necessary or may be delayed. Such measures include:
- physical therapy.
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- corticosteroid injections
What are the alternative options to shoulder replacement?
A shoulder arthroscopy procedure is frequently recommended people who have shoulder conditions that involve the surrounding ligaments, muscles and tendons, such as a rotator cuff injury or torn shoulder labrum. Arthroscopy is among the most common type of shoulder surgeries, and is attractive to many patients because it is minimally invasive. However, arthroscopic surgery primarily treats conditions that cause arthritis, rather than the arthritis itself. This treatment is generally useful in patients who do not yet have bone-on-bone arthritis.
How is shoulder replacement done?
In traditional shoulder replacement surgery (also known as "anatomic shoulder replacement"), the damaged humeral head (the ball of the shoulder joint) is replaced with a metal ball, and the glenoid cavity (the joint socket) is replaced with a smooth plastic cup, similar to that in a total hip replacement. More recently, a different type of surgery called reverse shoulder replacement was introduced to benefit patients who had a current or prior rotator cuff tear. (Find a surgeon at HSS who performs shoulder replacement.)
This metal-on-plastic implant system (rather than metal-on-metal) is used in virtually all shoulder replacement. In some patients, such as those with severe shoulder fractures of the humeral head, a partial shoulder replacement (called hemireplacement) may be recommended. This technique replaces the ball component only.

Figure 2: Anatomy of the shoulder, showing the implants after surgery.


Figure 3 (left): X-ray showing a traditional total shoulder replacement. Figure 4 (right): The Comprehensive Primary Shoulder System designed by HSS surgeons.
Anesthesia
During a total shoulder replacement, the patient may have either regional anesthesia with interscalene block or general anesthesia – or both. During the operation, the patient will be positioned sitting upright and partially or completely sedated.
Surgical steps of a conventional (anatomic) shoulder replacement
A traditional shoulder replacement surgery is composed of the following six basic steps:
- The surgeon separates the deltoid and pectoral muscles to access the shoulder in a largely nerve-free area (to minimize nerve damage).
- The shoulder is opened by cutting one of the front muscles of the rotator cuff, which covers the shoulder. This “opens the door” to allow the surgeon to view and manipulate the arthritic parts of the shoulder ball and socket.
- The arthritic sections of the joint are removed.
- The implant socket, ball and stem components are inserted. The metal ball component is attached to the stem, which extends down inside the patient’s humerus.
- The incision of the rotator cuff muscle is closed and stitched.
- The external (skin-level) incision is cleaned and stitched, and a bandage applied as a temporary covering.
Video: Conventional shoulder replacement animation
HSS surgeons have led the design of both conventional and reverse shoulder replacement implants. In 2023, an HSS surgeon implanted the world’s first stemmed elliptical head prosthesis for anatomic shoulder replacement, which was designed to facilitate conversion to a reverse shoulder replacement in the future, if needed by the patient.
Types of shoulder replacement implants
All shoulder replacement systems share the same basic components: a metal ball that rests against a plastic (polyethylene) socket. But their designs vary.
In anatomic shoulder replacements
The polyethylene socket in a traditional shoulder replacement is often cemented to the bone surrounding it, at least in part, so that fixation to the bone is immediate. The prosthetic ball has a stem that is usually placed inside the humerus without the need for cement. In most cases, the design of the stem prosthesis promotes, osseointegration, in which the patient's natural bone grows into the prosthetic material.
Surgeons from Hospital for Special Surgery designed a special implant called the Comprehensive Primary Shoulder System (see Figure 4), with a cobalt-chrome or titanium ball and a titanium stem. The system's specialized ball component creates a new humeral head that conforms to the patient’s exact anatomy. The ball, stem and socket all fit together in ways that provide a more customized fit. (Find a surgeon at HSS who performs total shoulder replacement.)
In reverse shoulder replacements
The components are still metal and plastic, but reversed: The metal ball is attached to the patient's existing socket, and a new plastic socket is attached to the patient's upper humerus, which formerly included the natural ball of the anatomic shoulder. Learn more about about reverse total shoulder replacement.
What are the risks and complications of a shoulder replacement?
Complications are rare in total shoulder replacement, but can include:
- instability (the ball slipping out of the socket)
- infection
- nerve damage
- glenoid loosening
- stiffness*
*An arthritic shoulder is often very tight prior to surgery. If, however, stiffness is still a problem in a shoulder in after motion was restored during surgery, this is usually the result of incomplete rehabilitation. Continuous physical therapy efforts are usually effective in restoring shoulder motion and strength.
How long does it take to recover from a shoulder replacement?
It generally takes eight weeks or more for patients to recover. It may be several months before a patient may do heavy labor or strenuous strength exercises.
On the day of surgery
The patient will wake up in the recovery room with the arm immobilized at the side in a removable canvass arm sling. Patients usually experience some temporary pain due to the surgery, but it is not the same type of pain they experienced due to their arthritis. Arthritic pain is largely absent from that point forward.
The day after surgery
X-rays will be taken to determine whether the implant is properly positioned. After the range of motion and stability of the implant are confirmed, physical therapy will begin that same day. Patients usually notice immediately that the shoulder is easier to move and the feeling grinding is gone.
The shoulder will be immobilized by a sling during the early rehabilitation phase to permit the tendons which have been repaired to heal. This sling is removable for showering and for rehabilitation exercises. Mobility improves throughout the period of physical therapy.
Timeline for complete recovery
Soon after surgery, the patient is permitted to use the hand and wrist. The usual timelines for complete recovery are as follows:
- Six weeks – The patient may use the whole arm, including shoulder, for light activity.
- Eight weeks (more in some cases) – The patient may begin unrestricted, active use of the arm and shoulder.
- Three months – Most patients are reasonably comfortable, have a range off motion about half of what is normal, and experience some weakness.
- Six months – Most patients are pain-free (although they may experience pain during certain weather conditions), and have motion and strength about two-thirds that of a normal level.
- One year – Approximately 95% of shoulder replacement patients will be pain-free. The remaining 5% will usually have no more than a weather-related ache or an occasional pain due to excessive activity. Likewise, there will probably not be significant strength limitations, depending on the condition of the deltoid and rotator cuff, particularly if both these muscle groups were normal before surgery.
Returning to work
The exact time a person can return to work depends greatly on the motion and strength of the shoulder and how the patient is progressing. Typically:
- Two to three weeks – Return to desk work is possible.
- Four months or more of recovery is required for heavier, physical labor.
The presurgical condition of the person's shoulder muscles and tendons play the largest role in the time frame of a patient’s recovery. If the muscles and tendons are in good shape prior to surgery, rehabilitation will be easier.
In all cases, proper and extensive postoperative rehabilitation are key factors in achieving the maximum benefit of shoulder replacement surgery.
Learn more about shoulder replacement surgery by exploring the additional content below, find a doctor at HSS who treats shoulder arthritis.
Additional content related to shoulder replacement
The videos in this series demonstrate the stages of rehabilitation you are likely to experience following a total shoulder replacement.
Shoulder Replacement Success Stories
In the news

