Blount's Disease: An Overview
- What is Blount's disease?
- What causes Blount's disease?
- How is Blount's disease diagnosed?
- How is Blount's disease treated?
What is Blount's disease?
Blount's disease (also known as Blount disease) is a form of bowleg deformity at or just below the knee joint. It is caused by an abnormality of the growth plate in one or more of the leg bones. It often appears in obese children and in young children who are early walkers. Blount's disease appears in children by two years of age. Its hallmark symptom is severe bowlegs.
Most commonly, the deformity is found at the top of the tibia (shinbone), the larger of the two bones in the lower leg. In these cases, the deformity occurs when the lateral (outer) side of the tibia continues to grow while the medial (or inner) side of the bone does not. Blount’s disease may affect leg only or both legs.

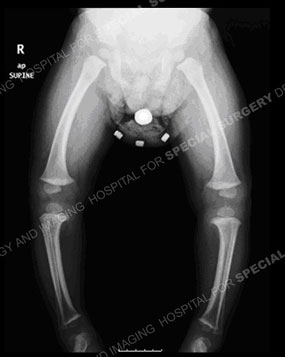
Figures 1 & 2: Photo and standing-alignment X-ray of a child with Blount's disease and bowlegs.
Left untreated, Blount's disease will not only worsen over time, but also create an increased risk of joint arthritis of the knee and other early degenerative changes.
What causes Blount's disease?
Causes of Blount’s disease include metabolic disorders such as rickets, renal (kidney) failure, infection, skeletal dysplasias (developmental abnormalities), and achondroplasia (a form of dwarfism).
How is Blount's disease diagnosed?
A diagnosis of Blount’s disease is based on a thorough patient history, physical examination and a standing-alignment X-ray in which an image of the leg – from hip to ankle. (See Figure 2.) The pediatric orthopedist uses this image to determine the mechanical axis of the deformity as well as its location.
How is Blount's disease treated?
Wearing braces may help children younger than three years, but surgery may be necessary in cases of failed brace treatment, delayed diagnosis or marked deformity at initial evaluation.
Nonsurgical treatment of Blount's: Bracing
The initial treatment for infantile or adolescent Blount’s disease is bracing, usually for a period of up to one year to determine effectiveness [Figures 3 & 4]. The standard bracing protocol involves use of a brace during waking hours with the knee in full extension during weightbearing. If gradual correction does not occur, surgery may be recommended. Results of surgery are much better before age four than after, when the recurrence rate of bowing goes up.


Figures 3 & 4: Photos of a child with Blount's disease in a brace.
Surgical treatment of Blount's disease
If the bowleg deformity is still present in the child after three years of age, and the angle of bowing is greater than 13 degrees as measured on a standing X-ray of the child’s lower extremities, surgery will be recommended.
Surgical procedures fall into two main categories:
- guided-growth surgery
- tibial osteotomy
Guided-growth procedure
Guided growth is the surgical approach usually used for treating children and teenagers with Blount’s disease. The guided-growth procedure is intended to correct further growth at the growth plate. Small metal plates are secured to the bone across the healthy side of the growth plate to stop the growth on that side of the tibia. This allows the effected, abnormal side of the growth plate to catch up. This progressive correction guides the growth of the leg in a way that straightens it.


Figures 5 & 6: Photos from the front and back of a child with bowlegs due to Blount's disease, prior to guided growth treatment.


Figures 7 & 8: X-rays of the same child before (left) and after (right) a guided growth surgical procedure. Note the plates used to fully correct the lower extremities in the knee area, outlined in white.


Figures 9 & 10: Photos of the child after surgery.
Tibial osteotomy
When guided growth fails to correct the deformity, and also in cases when the patient is already nearly or fully grown at the time of diagnosis, a different routine procedure called a tibial osteotomy may be required. In this procedure, the tibia bone is cut just below the knee joint, realigned to a corrected position, and a plate or external device is placed on the leg until the bone has healed into a straightened position.
Adolescent patients (teens) with Blount’s disease often also have some type of limb length discrepancy, which may also require surgical correction.


Figures 11 & 12: Photo and X-ray of a child with Blount's disease prior to a tibial osteotomy surgical procedure.


Figures 13 & 14: Photo and X-ray of the same child after a tibial osteotomy surgical procedure.
External fixators
If the correction is gradual, a circular fixator (also called a spatial frame) is used. This frame is also used when additional procedures are done simultaneously to correct other deformities such as a limb length discrepancy. The latter can develop when Blount’s disease affects only one leg. Due to the correction occurring in a gradual manner, the leg alignment may be fine-tuned. If the deformity correction is not perfect on an X-ray, correction can continue it until it is. The fixator is worn for between 8 and 12 weeks as the leg heals.

Figure 9: External Fixator
For additional information on External Fixation, see the Guide to Pediatric External Fixators (PDF).
Rehabilitation: Physical therapy for Blount's disease
Physical therapy is an important part of treatment, and most patients continue to see their rehabilitation therapists three times a week after leaving the hospital. Physical therapy helps ensure that the surrounding soft tissues remain flexible as the bone heals, and that muscle strength is maintained.
Updated: 8/5/2021
Images by the HSS Department of Radiology and Imaging
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Orthopedic Surgery, Weill Cornell Medical College


