Imaging for Osteoarthritis: An Overview

Osteoarthritis: A common joint disorder
Osteoarthritis (OA) is one of many different types of arthritis that can affect the human body. “Arthritis” comes from the Greek word arthron, meaning “inflammation.” However, this definition is not fully descriptive of the degenerative nature that osteoarthritis has on the knee, hip, shoulder, and other joints throughout the body.
Osteoarthritis is the most common form of arthritis, and is commonly associated with degeneration of articular cartilage, thickening of the bone under the cartilage (sclerosis), the presence of inflammation, and other features that are associated with joint destruction and deformity. The terminology of “degenerative joint disease” (DJD) may be used to convey a more accurate description of the whole joint degenerative nature of OA which has been historically associated only with the cartilage within a joint.
OA commonly affects the hip, knee, shoulder, the big toe, and the base of the thumb, and is commonly classified as primary or secondary OA. Primary OA is when the source of OA is unclear, and is commonly associated with age, sex, body mass index (BMI), or genetic factors. Secondary OA often has a clear source of joint degeneration and is commonly associated with joint injury, such as a trauma or repetitive-stress or occupational injury. Articular cartilage degeneration and other features of OA commonly occur as a gradual process.
Acquiring a radiograph (X-ray image), is a standard method your clinician will use to determine the stage of OA within a joint. The radiologist who interprets the image will use the description and gradation of osteoarthritis ("localized” or “diffuse" and "mild,” “moderate” or “severe," etc.), and this description will be used by your physician or surgeon to determine the best treatment options. Treatments include conservative, nonsurgical therapy, or surgery.
- Nonsurgical treatments can include physical therapy, modifications to physical activity, oral medications and/or intra-articular steroid injections
- Surgical options include osteotomies or joint replacement.
What are the different types of imaging examinations for osteoarthritis?
Conventional radiographs – Routine X-ray examinations
Regardless of the joint that is affected, conventional radiographs (X-rays) are used to evaluate your joint for osteoarthritis. The presence of osteoarthritis is displayed on the radiograph as a narrowing or a reduction in space between the bones of the joint where the cartilage has worn away, as well as by the formation of osteophytes (bone spurs) on the margins of the joint.

Anteroposterior (front to back) X-ray image of the knee showing osteoarthritis. Note the narrower spacing on the right side of the image, where cartilage has degenerated.
Schedule an X-ray at HSS. (A prescription is required.)
When cartilage is lost, bone rubs against bone. This can cause cysts or fluid-filled cavities in the bone, which will also be visible in an X-ray. The bone also responds with sclerosis (increased bone density), in which more bone grows under where the cartilage used to be. If the joint surfaces become misaligned, then osteophytes may form. There are basic routine X-ray views for imaging each joint:
- An anteroposterior (AP) view (front-to-back view)
- A lateral (outer side) view
- One or two oblique (45-degree) views
In order to detect early cartilage wear, HSS uses special X-ray views in place of or in addition to these standard views. These specialized views are designed to increase the sensitivity of a conventional radiographic study.
What kinds of specialized imaging can help diagnose osteoarthritis?
Symptoms of osteoarthritis may arise before the degeneration can be seen on standard X-rays. For this reason, radiologists at Hospital for Special Surgery often use the more sensitive MRI, CT and ultrasound forms of imaging, which are superior for detecting early osteoarthritis.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging is very sensitive imaging that can reveal subtle changes in bony and soft tissues. An MRI can show reactive bone edema (fluid build-up in the bone marrow), inflammation of soft tissues, as well as degenerated cartilage and damage to other soft tissues associated with OA. HSS uses a protocol of MRI pulse sequences with high sensitivity and accuracy to identify early evidence of cartilage degeneration. When evidence of cartilage generation is detected early, appropriate treatment can begin to minimize further degeneration, possibly postponing or eliminating the need for surgery.
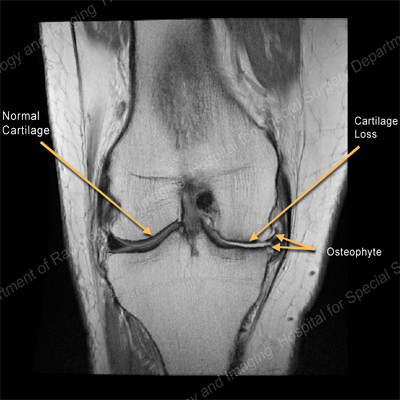
MRI of the knee showing normal cartilage on one side and cartilage loss and an osteophyte on the other.
Schedule an MRI exam at HSS
(A prescription is required)
CT scans
CT examinations, also called CT scans (or “CAT scans”), are excellent for showing bones and osteophytes (bone spurs). CT examinations are also useful in providing guidance for therapeutic and diagnostic procedures.

CT scan of an arthritic hip showing bony femoral head debris
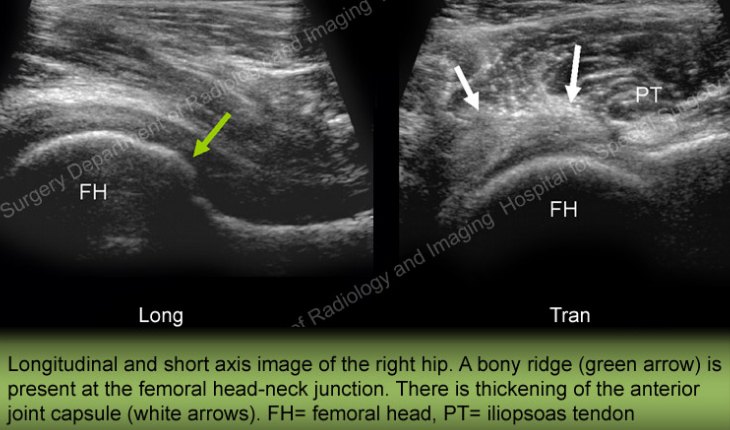
Ultrasound
Ultrasound is extremely sensitive for identifying synovial cysts that sometimes form in joints which have osteoarthritis. It is also excellent for evaluating the ligaments and tendons around the joint.
Schedule a CT scan or ultrasound at HSS. (A prescription is required.)
Interventional radiology: Radiographic-guided procedures
In addition to helping diagnose osteoarthritis, radiographic technologies can also be used to guide your doctor while applying treatments. For example, anesthetics and/or corticosteroids injected into a joint can help reduce the pain of osteoarthritis. It is helpful to perform such injection procedures using image guidance to aid in positioning the needle tip into the joint space. This kind of direct visualization can be performed using CT, ultrasound or fluoroscopy (a continuous real-time X-ray that works like an X-ray movie).
Arthrogram: A joint injection performed under fluoroscopic or CT guidance is called an arthrogram. The radiologist will inject a small amount of contrast agent into the joint to better visualize it. With ultrasound, the radiologist directly visualizes the needle inside the joint, as well as neighboring muscles, arteries and veins.
The faculty members of the HSS Department of Radiology and Imaging at HSS are board certified radiologists with specialized fellowship training in musculoskeletal imaging and cross-section imaging (MRI, CT, and ultrasound). Although other types of subspecialty physicians perform some of these procedures, radiologists are doctors who are trained in the use of all forms of imaging. HSS radiologists also have specific training in the physics behind the imaging, the safe use of ionizing radiation (fluoroscopy/CT), as well as in MRI and ultrasound safety.
What is the imaging process for hip and knee osteoarthritis?
Hip joint imaging
Standard X-rays of the hip
- The standard, conventional radiographic views obtained when a patient has hip pain from osteoarthritis are the anteroposterior (front-to-back) and lateral (outer side) view. A view of the pelvis is usually ordered at HSS as part of the initial examination to visualize other potential sources of hip pain, such as the low back or sacroiliac joints.
- Positioning for these views is very specific, as reproducibility is needed to follow progression of the condition, response to treatment and/or for preoperative planning.
Additional, optional X-rays of the hip
Optional radiographs are obtained routinely by HSS joint replacement surgeons. They include the Lowenstein lateral, cross-table lateral, false-profile and elongated femoral neck views. All of these views help to identify the precise site of osteoarthritis.
Common findings of hip osteoarthritis from X-rays
- Joint space narrowing is focal in the superolateral direction, apical (up and into the pelvis) or medial (into the center of the midline).
- As cartilage loss becomes severe, bone cysts and sclerotic remodeling (increased density of bone to fill the space formerly occupied by cartilage) is evident on the radiographs.
- Osteophytes (bone spurs) form opposite to the direction of cartilage loss and joint space narrowing. The osteophytes form in an attempt to stabilize the joints and compensate for the cartilage loss and narrowed joint space.
Knee joint imaging
Standard X-rays of the knee
The standard X-ray examinations obtained to evaluate knees with osteoarthritis are:
- Anteroposterior view (front-to-back view). At HSS, this view is usually obtained with the patient standing and bearing weight on the joint.
- Lateral (outer side) view.
- Merchant view of both patellofemoral joints (top-angled view, looking down at the knee caps).
Additional, optional X-rays of the knee
Optional radiographs are routinely ordered at HSS. Most often, these will be a posteroanterior (back-to-front) X-ray, taken while the knee is weightbearing (standing position) and in slight flexion (knees slightly bent). This position helps the radiologist evaluate whether there is cartilage loss in the posterior (rear) portion of the of the medial (inside) or lateral (outer side) knee joint compartments. Positioning for these views is very specific.
Common findings of knee osteoarthritis from X-rays
Typically, the cartilage in one compartment of the joint (that is, the medial, lateral, or anterior patellofemoral joint compartment) is most severely affected. The standing X-rays may show narrowing of the involved joint space of the knee. Altered alignment of the knee joint is very common as either the cause or as a result of osteoarthritis. The patellofemoral joint (at the front of the knee) can be the focus of osteoarthritis of the knee or part of a more generalized condition. Lateral subluxation or patellar malalignment is very common.
As the disease progresses, osteophytes form along the joint margins and bone cysts and sclerosis are typically present. When osteochondral or cartilage fragments break off, they can remain in the joint or can get larger and are referred to as intra-articular loose bodies. Fluid can form in the joint secondary to the arthritis and is referred to as an effusion.
Updated: 3/21/2024
Authors
Department of Radiology and Imaging
Hospital for Special Surgery
Related articles
Reviewed by Matthew F. Koff, PhD
Assistant Scientist, Department of Radiology and Imaging, Hospital for Special Surgery
Assistant Professor of Biomedical Imaging in Orthopaedic Surgery, Weill Cornell Medical College