Osteoarthritis
Osteoarthritis is the most common form of arthritis.
What is osteoarthritis?
Osteoarthritis (OA) is a painful condition involving the deterioration of a joint. It affects primarily the cartilage but also the surrounding structures of the entire joint, including tendons, ligaments, and bone. Affecting 32 million people in the United States, OA is the most common joint disease in the world.
What causes osteoarthritis?
Most often, OA develops in people over age 50. However, younger people may get the condition early as a result of an injury (such as a fracture, dislocation, or tendon/ligament damage). It can also result from abnormal formation of the joint in the womb or as a child. Being overweight can lead to more stress on the joints, particularly the knee, and higher rates of osteoarthritis.
What is the difference between osteoarthritis and rheumatoid arthritis?
Unlike OA, rheumatoid arthritis rheumatoid arthritis is a chronic disease of the immune system which causes inflammation in the joint when tissues lining the joints are recognized as foreign. Sometimes, both rheumatoid arthritis and OA can be seen in the same joint.
Which joints are most commonly affected by arthritis?
The joints most commonly affected by osteoarthritis are the:
- hips
- knees
- basal joint at the bottom of thumb
- neck (joints of the cervical spine)
- lower back (joints of the lumbar spine)
- ankles
- feet
What are the symptoms of osteoarthritis?
Joint pain is the most common symptom of OA. It typically increases with activity and decreases with rest. Stiffness is also a symptom of osteoarthritis. It is often present in the morning, and usually lasts for less than 30 minutes. It can also occur during the day when a patient sits for a period of time “gelling” and improves quickly when the person stands or walks. Pain felt during movement of the joint is often accompanied by a crackling or grinding sound called "crepitus." These sounds can sometimes be heard in joints of people without severe OA as they reflect the bones, tendons and ligaments changing position as the joint moves.
Some people with severe OA damage seen on X-ray images have little pain or impaired joint function, others have severe pain and disability despite mild imaging changes. The level of pain each person with OA experiences depends on many factors, such as genetics, body weight, previous injury, and psychosocial factors. OA is typically not associated with significant swelling, redness or warmth in the joints, fever, or unexplained weight loss. These symptoms are consistent instead with forms of inflammatory arthritis.
How is osteoarthritis diagnosed?
The key elements to getting an accurate diagnosis for osteoarthritis are:
- a complete evaluation of patient history and physical examination by a doctor
- laboratory tests to rule out other causes of arthritis
- imaging, such as X-ray films
The history and physical examination
An accurate medical history and physical exam is crucial to the diagnosis of osteoarthritis. This includes information about:
- pain levels
- joint range of motion
- muscle strength in the affected region
- presence of any swelling or tenderness of the joint
- gait (the way you walk), if the disease is in the lower half of your body
Laboratory tests for osteoarthritis
When the physical exam suggests a person may have osteoarthritis, different forms of imaging may be necessary to confirm the diagnosis and determine the severity of the joint degeneration.
- complete blood counts
- uric acid levels
- metabolic profile
- urinalysis
- markers of inflammation (such as CRP or erythrocyte sedimentation rate) rheumatoid factor or anti-CCP (to detect rheumatoid arthritis)
- antinuclear antibody (ANA) titer tests
When these tests are normal or return negative results, it suggests that joint pain is not due to one of these conditions. However, doctors do not rely on laboratory tests alone, but the medical history, physical exam, and imaging. Another test that may help confirm the diagnosis is the extraction and analysis of fluid from the joint (synovial fluid). This fluid helps nourish and lubricate the joints and is usually present in very small amounts. However, when certain forms of arthritis are present, the amount of synovial fluid can increase, and its composition can change. The fluid may also be examined for the presence of crystals seen in gout or similar conditions.
Radiological imaging for osteoarthritis
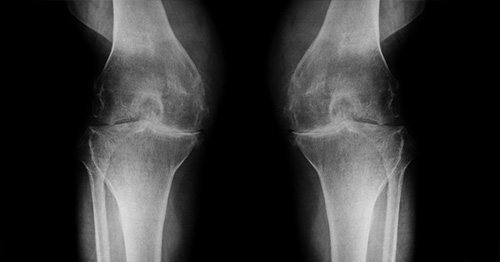
While imaging of the joint is not always required for a clinical diagnosis of OA, different forms of imaging are often helpful. In later stages, OA can be seen on X-ray images.
However, X-ray images do not show the early changes in a joint associated with OA or in the tissue surrounding the joint. These changes typically require other imaging techniques, such as MRI, CT scan, or ultrasound can be useful to accurately evaluate the structures in the joint.

Anteroposterior (font-to-back) X-ray showing severe, late-stage OA of the right hip joint (seen on the left side of the image)
- MRI (magnetic resonance imaging): This can reveal subtle, early changes in bony and soft tissues of the joint.
- CT scan (computed tomography, sometimes called a "CAT scan"): A CT exam is excellent for showing the formation of osteophytes (bone spurs) and how they affect the surrounding soft tissues of the joint.
- Ultrasound: This is useful for identifying characteristics of OA at the bedside or in patients who cannot have an MRI exam because of certain medical conditions.
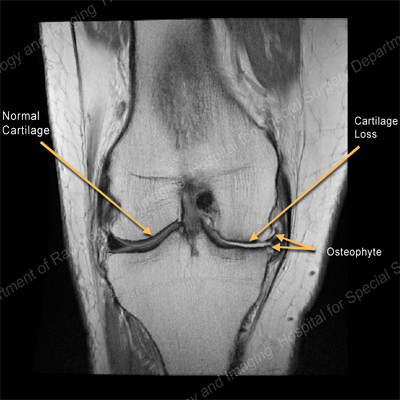
MRI of the knee showing normal cartilage on one side and cartilage loss and an osteophyte on the other.

MRI of the hip demonstrating osteoarthritis with large osteophytes around the femoral head.
How is osteoarthritis treated?
Your doctor will develop an individualized treatment program especially for you based on several factors, including:
- the severity of your pain
- how much your function is affected
- what treatment approaches have been tried (for example, physical therapy, medications, injections)
which joints are involved - your other medical conditions
- your preferences and goals for treatment
What are the nonsurgical options for treating osteoarthritis pain?
The first line of treatment for osteoarthritis typically involves physical and occupational therapy. HSS has therapists who apply cutting edge techniques to our patients according to their needs. Weight loss, exercise, and self-management programs are also frequent components of OA. Staying active is essential.
For people with osteoarthritis, it is important to maintain an active lifestyle and avoid becoming sedentary. Movement can help reduce pain and prevent it from getting worse. The appropriate and safe types of activity vary from patient to patient. As with any treatment, getting a proper “movement prescription” requires getting an accurate, pinpointed diagnosis and ensuring that all members of the healthcare team (medical specialist such as a rheumatologist, physiatrist, an orthopedic surgeon, a physical therapist, etc.) understand each patient's unique condition.
To reduce the effects of early-stage OA of the knee, it is especially important to strengthen the thigh muscles to provide better support for the joint during walking and other activities Balance training can also help maintain muscle strength and project the joint from further damage.
Oral medications for osteoarthritis
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat OA. Examples include ibuprofen (Advil), naproxen (Aleve) and celecoxib (Celebrex). Duloxetine (Cymbalta) is a medication used to treat anxiety and depression, but which has also been shown to alleviate OA pain.
Joint Injections for osteoarthritis
Depending on the joint involved, injections of corticosteroids, or hyaluronan-containing compounds may be used to reduce the pain of OA.
When should I consider surgery?
When the measures above are not enough and pain in a specific joint makes it difficult for you to function in the ways that you want then joint replacement surgery can restore your comfort and help you to return to normal activity. Hip replacement surgery and knee replacement surgery have become trusted treatments for restoring mobility and easing pain.
For cases of hip arthritis or knee arthritis, some patients may be able to have less invasive hip arthroscopy or knee arthroscopy procedures. Joint replacement surgery may also be an option for people with arthritis of the shoulder, elbow, wrist or ankle.
You are generally a good candidate for surgery if you have tried the treatments above, but they have not worked and you are experiencing significant impairments in your daily life – joint pain is waking you up at night, or you are not able to participate in activities with family and friends. These impairment can often lead to depression, which can make the pain seem even worse. In addition, people often decrease their activity so that their joints hurt less. However, although this might prevent joint pain, this strategy can lead to weight gain, and increase the risk for high blood pressure, diabetes, and even heart attack. In such cases, surgery is a reasonable consideration. The exact type of surgery you have will depend on your age, activity level, and the specific joint that is affected.
HSS research enhances arthritis treatment options
Hospital for Special Surgery’s pace-setting medical research contributes essential knowledge to researching the prevention and treatment of osteoarthritis and inflammatory arthritis. Learn more about OA research at HSS:
- Biomechanics Research
- Bone Health and Spine Regeneration
- Integrated Spine Research Program
- Laboratory of Molecular Osteoarthritis Research
Learn more about OA from the articles below.
Articles on osteoarthritis
Learn more about the basics of osteoarthritis from HSS expert physicians.
Articles related to osteoarthritis treatments
Get in-depth information on numerous surgical and nonsurgical treatment options for osteoarthritis.
Articles on osteoarthritis prevention
Read more about risk factors for osteoarthritis and how different injuries and activities may affect them.
Articles on osteoarthritis wellness
Get tips on how to manage pain and stiffness when you have osteoarthritis.
- What to Know About Joint Pain: Types, Causes and Treatments
- The Best Types of Exercise for Sore Knees
- Best Bet Exercises for Osteoarthritis of the Shoulder
- Best Bet Exercises for Osteoarthritis of the Spine
- Assistive Devices for Arthritis of the Hands: Protecting Your Joints
- Guidelines to Help Reduce the Side Effects of NSAIDs (Nonsteroidal Anti-inflammatory Drugs)
- Guidelines to Help Reduce the Side Effects of COX-2-Specific Drugs Like Celecoxib (Celebrex)
Osteoarthritis Success Stories
References
- * (statistic reference) https://www.cdc.gov/arthritis/basics/osteoarthritis.htmAiyer R, Noori S, Schirripa F, Schirripa M, Aboud T, Jain S, Gulati A, Puttanniah V, Gungor S, Hunter C. Treatment of knee osteoarthritic pain with platelet-rich plasma: a systematic review of clinical studies. Pain Manag. 2021 Apr;11(4):419-431. doi: 10.2217/pmt-2020-0052. Epub 2021 Mar 25. PMID: 33764185.
- Cole BJ, Gilat R, DiFiori J, Rodeo SA, Bedi A. The 2020 NBA Orthobiologics Consensus Statement. Orthop J Sports Med. 2021 May 6;9(5):23259671211002296. doi: 10.1177/23259671211002296. PMID: 34017878; PMCID: PMC8114275.
- McLeod MM, Kim JS, Moley P, Fontana MA, Blevins J, Chalmers B, Bamman M, Bostrom MP. Arthritis Foundation/HSS Workshop on Hip Osteoarthritis, Part 4: Nonoperative Options, Machine Learning in Predicting Total Hip Arthroplasty, Robotics, and Phenotyping to Guide Precision Rehabilitation. HSS J. 2023 Nov;19(4):473-477. doi: 10.1177/15563316231193367. Epub 2023 Aug 17. PMID: 37937083; PMCID: PMC10626938.
- Zahir H, Dehghani B, Yuan X, Chinenov Y, Kim C, Burge A, Bandhari R, Nemirov D, Fava P, Moley P, Potter H, Nguyen J, Halpern B, Donlin L, Ivashkiv L, Rodeo S, Otero M. In vitro responses to platelet-rich-plasma are associated with variable clinical outcomes in patients with knee osteoarthritis. Sci Rep. 2021 Jun 1;11(1):11493. doi: 10.1038/s41598-021-90174-x. PMID: 34075069; PMCID: PMC8169703.
Updated: 12/5/2023
Reviewed and updated by S. Louis Bridges, Jr., MD, PhD; and Lisa A. Mandl, MD, MPH