Orthopedic Complications of Neurofibromatosis Type 1: Scoliosis, Tibial Dysplasia and Other Issues

- What is neurofibromatosis?
- How is neurofibromatosis type 1 diagnosed?
- Neurofibromatosis type 1, scoliosis and kyphosis
- Neurofibramotosis type 1 and bowing of the tibia
- Looking to the future
What is neurofibromatosis?
Neurofibromatosis is a genetic disorder characterized by tumors known as neurofibromas, which grow in the nervous system and under the skin. This disease occurs as two distinct types: neurofibromatosis type 1 (NF1), which is more common, and neurofibromatosis type 2 (NF2).
NF1 affects about one in every every 3000 people. NF2 affects only about one in every 25,000 people. NF2 does not frequently cause orthopedic problems. For this reason, this article focuses on issues related only to NF1.
Neurofibromatosis type 1
In addition to the neurofibroma skin lesions and discoloration, children with NF1 frequently also develop orthopedic problems, according to Roger F. Widmann, MD, Chief of Pediatric Orthopedic Surgery at Hospital for Special Surgery (HSS). The two most common are spine deformities, particularly scoliosis − a lateral (sideways) curvature of the spine − and tibial dysplasia, in which the tibia (shin bone) fails to develop appropriately. Patients with tibial dysplasia may be more susceptible to fractures and to develop pseudarthrosis, in which the broken tibia heals improperly. Tibial dysplasia can also result in limb length discrepancy, where one leg is longer than the other. Other children with NF1 may develop a larger and longer leg without having any underlying bone problems. In these cases, the cause is overgrowth of soft tissues in the limb.
NF1 is associated with “acoustic neuromas” that may affect a person’s hearing and balance.
How is neurofibromatosis type 1 diagnosed?
A diagnosis of neurofibromatosis type 1 is made in children with two or more of the following criteria:
- skin lesions (neurofibromas)
- multiple spots on the skin that are darker than a patient’s normal skin tone (sometimes called “café au lait” spots because on people with lighter skin tones, they are similar in color to coffee with milk)
- freckling in the groin and underarms, eye abnormalities, including lisch nodules (tiny pigmented tumors in the iris)
- particular skeletal abnormalities such as scoliosis or tibial dysplasia
- a family member with NF1


“Café au lait” spots (left) and axillary freckling of the underarm (right)
In cases where diagnostic findings are not conclusive, but neurofibromatosis is suspected, the child should be closely monitored by a multidisciplinary team that includes a pediatric neurologist and a geneticist.
Neurofibromatosis type 1, scoliosis and kyphosis
Children with NF1 who develop scoliosis may be diagnosed with either dystrophic (degenerative) or nondystrophic forms of scoliosis. Dystrophic scoliosis worsens quickly and unrelentingly.
Nondystrophic scoliosis symptoms and treatments
The condition resembles adolescent idiopathic scoliosis, with similar types of curves and curve patterns.
Treatment for nondystrophic scoliosis can include bracing as well as surgery. Instrumentation is used to realign the spine, and bone grafting is performed to help achieve spinal fusion. While the health risks associated with nondystrophic scoliosis are less pronounced, these curves can modulate into dystrophic scoliosis over time and therefore need to be monitored carefully until the child reaches maturity.


Posteroanterior (back-to-front) X-rays of dystrophic (first image) and nondystrophic scoliosis (second image)
Dystrophic scoliosis symptoms and treatments
“In cases of dystrophic scoliosis, we typically see shorter, more sharply angulated curves,” Dr. Widmann says. Characteristics of dystrophic scoliosis also include several bone abnormalities, including thinning of the ribs, significant rotation of the vertebrae, vertebral wedging, and erosion of the vertebrae by the spinal fluid, owing to the poor quality of the bone. Dystrophic scoliosis is also associated with kyphosis or a forward tilt of the spine, which can progress rapidly and may result in impingement of the spinal cord.
Due to the risks associated with NF1, orthopedic surgeons usually recommend surgery at a smaller curve magnitude (between 20 and 40 degrees) than with nondystrophic scoliosis. In contrast, surgery is recommended for idiopathic scoliosis patients with curves that exceed 50 degrees. Bracing is usually not an option in cases of dystrophic scoliosis.
“Surgery to correct a dystrophic scoliosis curve can present special challenges, including the need to correct a kyphotic (rounding of the back) curve at the same time,” Dr. Widmann explains. These surgeries also carry a risk of pseudoarthrosis or non-union. To help minimize this risk, Dr. Widmann and his colleagues at HSS use a graft from the patient’s iliac crest bone (part of the pelvis) to achieve the fusion, as opposed to the allograft often used in other scoliosis surgeries. These complicating factors often necessitate more than one surgery.
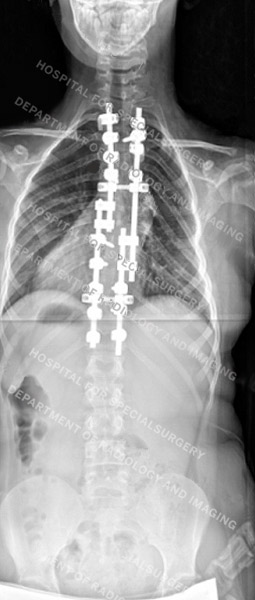

Posteroanterior (back-to-front) X-rays of dystrophic scoliosis (first image) and nondystrophic scoliosis (second image) after surgery
Neurofibramotosis type 1 and bowing of the tibia
Unlike the benign bowing of the legs that is not uncommon in healthy young children, the bowing of the tibia that is associated with neurofibromatosis has a distinctive orientation − an anterolateral bow (see figure below). This may lead to fracture and tibial pseudarthrosis (non-union) In such cases, surgical intervention is recommended.

Anteroposterior (front-to-back) X-ray showing an anterolateral bowing in the tibia of a young patient
Looking to the future
While there is no cure for neurofibromatosis, careful monitoring and intervention for orthopedic and other complications improve the patient’s quality of life significantly
Learn more about the Pediatric Orthopaedic Service.
Updated: 6/4/2021
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Professor of Clinical Orthopedic Surgery, Weill Cornell Medical College
Associate Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Orthopedic Surgery, Weill Cornell Medical College

