Minimally Invasive Bunion Surgery
A bunion (hallux valgus) is a condition in which your big toe has a protruding bump at its base on the inside of the foot. This bump occurs when your foot alignment changes and causes your big toe to move toward the smaller toes. Pain can occur as a result of pressure from the bump against your shoe and/or if your big toe rubs against your second toe. In addition, pain can sometimes occur in the ball of the foot as a result of the big toe's poor alignment.
Can bunions be corrected without surgery?
Conservative, nonsurgical treatment for bunions include wearing only wide-toed and/or soft shoes, using “bunion pads” or toe spacers, and taking nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. Toe spacers and devices to hold the big toe apart from the second toe may help with pain, but they will not make the bunion go away. The alignment of the toe will not get better over time without surgical intervention.
Who should have bunion surgery?
Bunion removal surgery should not be done for cosmetic purposes only. It is performed on patients whose daily lives are affected by pain and difficulty wearing shoes even after trying wider, more comfortable footwear.
If you have tried wearing wider shoes, padding, toe spacers or other treatments but still have pain that is limiting your activity, you may be a candidate for surgical bunion correction.
What is the surgery for bunion correction?
The corrective surgery for bunion is known as a metatarsal osteotomy or bunionectomy. There are multiple techniques, but all involve cutting the bones and repositioning them with metal screws to straighten the big toe and reduce the bump on the side of the foot.
Traditionally, bunion surgery can be quite painful and involve a long recovery. However, some patients can benefit from newer, minimally invasive techniques that have significant advantages. Historically, these procedures have been performed through large incisions, but at HSS, I have perfected two special techniques to correct bunions through tiny incisions.
How does minimally invasive bunion surgery work?
Minimally invasive bunion surgery is performed using a burr, instead of a saw, to cut the bone. This allows the cuts to be made “percutaneously,” or through tiny incisions made through the skin of the foot, instead of the long incisions most often used in traditional techniques.
By avoiding large incisions, fewer soft tissues (skin, muscle, joint capsule, etc.) are disrupted, so the foot is less swollen and painful after surgery. This allows for immediate weightbearing, faster bone healing and a quicker return to baseline activity levels. I perform two types of minimally invasive bunion correction, depending on the severity of a patient’s bunion:
- For mild to moderate bunions, I use the PECA, or Percutaneous Chevron Akin, technique. This involves cutting the first metatarsal bone and the big toe bone, repositioning them to correct the alignment
- For severe bunions, I perform the (minimally invasive, or MIS) Percutaneous Lapidus technique. This involves repositioning and fusing a joint closer to the arch and also cutting the toe bone. We are able to correct the bunion in all three planes (including rotation) using my own developed technique. While most surgeons use a large incision, a saw, and large plates for this type of correction, I use a burr and place screws through tiny incisions. Similar to the PECA technique, this surgery also allows early weightbearing with less pain, a better cosmetic outcome, and faster return to work and sport.
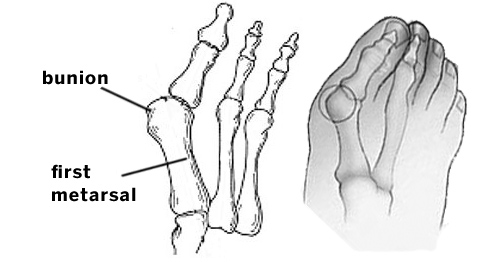
Illustrations of foot anatomy showing location of a bunion and the first metatarsal bone.
What are the benefits of minimally invasive versus open bunion surgery?
Minimally invasive bunionectomy involves less pain, a faster recovery, and better cosmetic results due to the small incisions. Open surgery, however, is a more powerful correction for very severe bunion deformities. It also reduces the risk of recurrence in severe bunions.
I have noticed that my patients who have the minimally invasive technique take less pain medication, have better range of motion of their big toe, and are back in regular shoes in half the time than are my patients who undergo the open technique.
Can I have minimally invasive bunion surgery?
This can be determined only through a physical examination of your foot. including seeing you stand, and assessing weightbearing X-rays of your foot. If you have a severe deformity associated with other foot problems that require surgical intervention, you may need a more involved, open procedure. It’s best to speak with your orthopedic foot and ankle surgeon to see which option is right for you.
How is painful is bunion surgery?
The bunion surgery I perform at Hospital for Special Surgery in New York City is not nearly as painful as traditional bunion surgery. All patients get a nerve block that numbs the foot for 24 hours after surgery. Patients are instructed to take ibuprofen and acetaminophen (Tylenol) for two to three days after surgery as well. Less than half the patients need stronger medication, and those who do take less than five pills.
When bunion surgery is performed as part of a larger foot surgery, the pain may be worse.
How long should you stay off your feet after bunion surgery?
For every foot surgery, patients should stay off their feet and rest for the first two weeks. Typically, it is recommended that you keep the surgical area elevated 80% of the time during the first week and 50% of the time in the second week. Depending on the type of correction you have, you will be allowed to put weight on your foot either after 24 hours (for the PECA surgery) or after two to four weeks (for the minimally invasive Lapidus surgery). Most patients take at minimum two weeks off from work unless they work from home, and longer if they have to commute by public transportation or drive.
How long does it take to recover from bunion surgery?
The full recovery period depends largely on whether you have minimally invasive or open surgery. Typically, minimally invasive surgery patients can walk in normal sneakers after about six weeks with the PECA procedure or eight weeks with the MIS Lapidus procedure (compared to 10 to 12 weeks after open surgery). From there, activity is increased as tolerated by the patient. Running and jumping are restricted for 12 weeks, but biking, spinning, walking and swimming are allowed to progress as the patient tolerates.
Recovery from minimally invasive bunion surgery
After PECA surgery, you will be fitted with a special surgical post-op shoe, and you can bear full weight almost immediately, after full feeling in your foot has been restored. For the first two weeks after surgery, you will need to limit your activity and keep your foot elevated about 50% to 80% of the time to decrease the swelling and allow the wounds to heal.
After the first two weeks, you may be given a bunion splint to maintain the postsurgical alignment. During this time, you can gradually increase your walking and resume normal activities of daily living.
How long after minimally invasive bunion surgery can I wear normal shoes?
You will continue to wear the special post-op shoe for about six weeks after surgery. Typically, you will be able to start wearing a normal sneaker after about six weeks, depending on your level of swelling and comfort. Most patients fit into flat, comfortable shoes and all sneakers and boots by three months postoperatively. Patients can experience some degree of swelling for 6 to 12 months after surgery that may limit high fashion shoe wear. This varies by individual, but if other surgery has also been performed on the foot, such as hammertoe corrections, the time it takes to get into regular shoes can increase. Typically, you will be able to wear a regular sneaker at about 10 to 12 weeks after surgery, and you can increase your activity as tolerated from there.
How successful are bunion operations and what are the risks?
The majority of patients are very happy with their bunion operation. Assuming the patient follows the postoperative instructions carefully, the outcomes are very good. There are risks of bunion surgery, however. Delayed bone healing can occur with any foot surgery, but this is rare. This risk is increased if patients do too much too soon (against the doctor’s advice) and/or they have health issues that can affect bone healing. Some numbness around the incisions may be noted after the procedure. This typically goes away in three to six months. In rare cases it can persist. Bleeding, blot clots, and risks associated with anesthesia are also rare complications. Recurrence of the bunion (the bunion coming back) can occur after any type of correction, and this risk is not known to be increased in those who have the minimally invasive bunion correction surgery.
Do bunions grow back after surgery?
The recurrence rate (a bunion coming back after surgery) is about 20% over a patient’s lifetime. A mild bunion recurrence is well-tolerated by most patients. Significant bunion recurrences that cause problems and require further surgery are much less common. Recurrence may happen if the bunion isn’t fully corrected at the time of surgery or if the wrong bunion procedure was used. It may also occur if patients don’t follow the postoperative directions carefully. Overcorrection (“hallux varus”) is also a risk, but much less common. Either recurrence or overcorrection may require a second operation (revision surgery).
How can you prevent a bunion from growing back?
Bunions are hereditary so certain conditions may make someone more prone to having the bunion come back. Any condition that causes hypermobility, or tissue flexibility, can be the cause of recurrence. If the bones don’t heal properly, the bunion can recur as well. Wearing sensible shoes (flat, comfortable) when possible may help maintain your bunion correction.
Posted: 1/20/2022
Authors
Associate Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Orthopaedic Surgery, Weill Cornell Medical College
Related articles
References
- Schipper ON, Day J, Ray GS, Johnson AH. Percutaneous Techniques in Orthopedic Foot and Ankle Surgery. Orthop Clin North Am. 2020;51(3):403-422. doi:10.1016/j.ocl.2020.02.004.

