Early Hip Conditions
Diagnosis and Non-operative Treatment
People suffering from severe hip-related debility and pain owing to advanced osteoarthritis, congenital defects, or trauma, are often treated with surgical procedures. But for most individuals with hip pain, a range of non-operative options can often alleviate pain and restore function.
In the healthy hip joint, the upper end of the femur (thighbone) meets the acetabulum, fitting together like a ball and socket. Articular cartilage, a smooth protective liner covers the bones and limits friction between the joint surfaces during movement, allowing the ball to rotate freely in the hip socket. Another piece of soft tissue called the labrum, which is made of fibrocartilage, lines the outer rim of the hip socket to create a suction seal that helps hold the ball-like femoral head in place.

Figure 1. Illustration showing the pelvis, acetabulum (hip socket), labrum, femoral head (ball of the hip joint) and surface of articular cartilage
Conditions affecting the hip that may respond well to non-operative care include, but are not limited to:
- Soft tissue injury including tendonitis and bursitis
- Labral tears – an injury to the labrum, a specialized piece of cartilage that runs along the rim of the hip socket. The labrum provides additional cushioning, a “suction effect” that helps hold the femoral head in place, and added stability to the hip joint
- Early osteoarthritis
- Mild hip dysplasia, a condition in which the acetabulum or cup portion of the hip joint is not fully developed
- Femoroacetabular impingement (FAI), a condition in which the femoral head or ball portion of the joint or the acetabulum do not fit normally in place, creating an incongruity or imperfect fit of the ball and socket joint.
- Other bony abnormalities
“While many patients exploring non-operative care do so as a first step in the treatment of their condition, non-operative treatment can also be a good option for patients who are not candidates for surgery,” explains Peter J. Moley, MD, assistant attending physiatrist, at the Hospital for Special Surgery’s Center for Hip Preservation. Patients treated at the Hip Center benefit from the availability and perspective of a multidisciplinary team that also includes orthopedic surgeons, radiologists, and physical therapists. “Together we’re able to evaluate each case and develop a treatment plan that’s in the best interest of the patient, whether that means initiating non-operative measures or going directly to surgery,” Dr. Moley says.
Evaluation and Diagnosis
Evaluation of hip pain begins with a complete history and physical assessment - including the patient’s range of motion, impingement signs, and strength. A full lumbar spine exam and assessment of neurologic function are also done. X-ray images of the painful hip are obtained. In some cases an MRI is also necessary.
With a complete work up, in most cases, the diagnosis can be made and the patient can begin rehabilitation. But in someinstances, the physician may administer a diagnostic injection into the hip joint or soft tissues. If the patient experiences immediate pain relief, the hip joint or soft tissues may be shown to be the source of the pain. If pain persists, it may originate from another part of the body such as the spine and the patients may require treatment for both areas.
Non-operative treatment options
Once the diagnosis has been established, the physiatrist works with patients to identify reasonable treatment goals, whether it’s a return to recreational running or being able to climb up the subway stairs.
For many individuals, activity modification offers the greatest benefit. A runner who switches from a regimen of 40 miles a week to half that amount, for example, often feels significantly better. While some dedicated athletes find this to be a difficult psychological adjustment, switching to spinning (an exercise that resembles riding a stationary “bicycle”) or water exercise can make the process of activity modification easier.
Physical therapy to strengthen the muscles that support the hip joint and increase range of motion is another essential component of non-operative care. The hip muscles reduce joint stress with each step a patient takes. Patients undergoing physical therapy are therefore advised on the importance of muscle strengthening exercise.
Because physical therapists outside the hospital have varied training and approaches to hip injury and disease, when possible, patients are encouraged to work with professionals at the HSS Center for Hip Preservation or individuals in the HSS network. “To standardize care, we offer a hip rehabilitation course to all network therapists. In this way we can ensure that care is consistent with what we find to be most effective,” explains Dr. Moley. Physical therapists may also address conditions affecting the lumbar spine if they are found to be associated with the patient’s pain.
Other adaptation/interventions include:
- The use of a cane on the opposite side of the painful hip – which can reduce stress on the joint by up to 30 percent.
- Weight loss, if necessary, since extra pounds place greater stress on the hip joint
- Use of a short course of oral nonsteroidal drugs (NSAIDs) for mild to moderate pain.
Therapeutic Injections/Epidurals
Patients who have persistent pain, even after activity modification and a regimen of physical therapy, may be candidates for a steroid injection into the joint or soft tissues. An alternative under investigation is viscosupplementation – injection with a substance that mimics naturally occurring synovial fluid that helps lubricate the joint. This has been shown in limited research to be effective for early hip arthritis.
Up until recently, physiatrists and other specialists have injected a steroid directly into the joint. However, good results can also be achieved with selective injection. With this technique, the physician places the steroid in the specific area that is inflamed and painful, such as a defined part of the capsule (the fibrous tissue that encloses the hip joint) or the ilio-psoas tendon, which runs outside the hip joint and is involved with flexion of the hip.
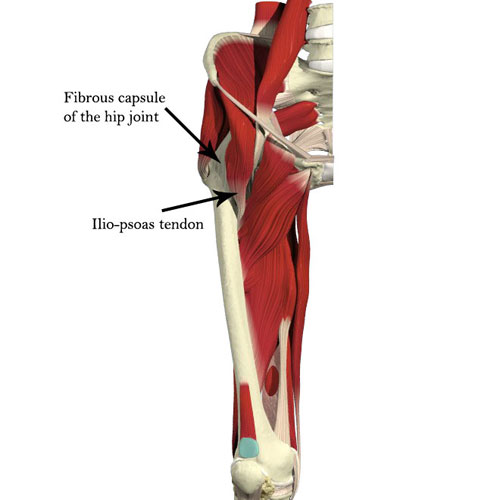
Figure 2. Illustration showing the hip capsule and important muscles around the hip including the ilio-psoas muscle and tendon
Because steroids can actually damage cartilage, their use is generally restricted to one or two injections into the joint; selective injection could reduce this risk.
At HSS, to ensure patient safety and for use as a future reference, all injections and epidurals are administered using ultrasound or fluoroscopic guidance and are documented on film.
Center for Hip Preservation: Looking to the Future
Patients seeking care for hip pain at institutions that do not specialize in hip care may not be informed of the entire range of treatment options available. At HSS, where large numbers of patients with hip disease and injury are treated every day, the multidisciplinary team is committed to educating patients on the full spectrum of available treatments, from physical therapy to surgery.
A patient with a labral tear, for example, should be assessed for mechanical derangement to determine the reason for the injury. For most patients, a trial of non-operative care and rest should be initiated before considering surgical repair.
At the Center for Hip Preservation, accumulating data that demonstrates the success of non-operative care is an important focus. To build this knowledge base, all patients are entered into a registry that carefully tracks their progress and the outcome of treatment. “Because non-operative care can involve multiple variables, and because we see our patients over a more limited period, results of these measures are harder to quantify than results achieved by surgery. But we’re making significant progress learning what works best for our patients and we’re going to learn a lot more over the next ten years. It’s an exciting time to be working in this area,” says Dr. Moley.
Authors
Associate Attending Physiatrist, Hospital for Special Surgery
Associate Professor of Rehabilitation Medicine, Weill Cornell Medical College
Related articles
Other resources
Summary by Nancy Novick.
